The quest for a longer-lasting whooping cough vaccine
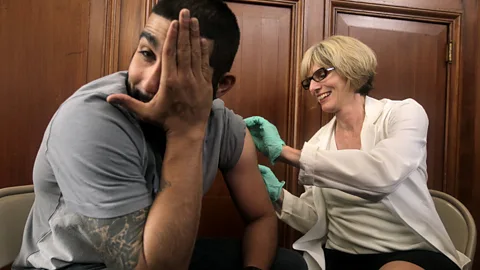
 Getty Images
Getty ImagesThis 19th-Century killer is making a comeback – and with protection from the whooping cough vaccine waning over time, the hunt is on for something longer-lasting.
Whooping cough wasn't really on Juliet Lautenbach's radar. During her pregnancy and her daughter's childhood, both had received free public vaccines against whooping cough along with all the other standard immunisations.
But five years after giving birth, Lautenbach was working in an open-plan office with a colleague who was coughing a lot. The coworker revealed that she had whooping cough, and Lautenbach realised that both her persistent cough and her daughter's could be related. Lautenbach doesn't blame that colleague, but notes that "for every person who walks around with whooping cough, there's somebody sitting within two desks of them in a closed office space who has a young child who's vulnerable".
Lautenbach, a civil servant and fantasy author based in Canberra, Australia, still remembers how intense the four weeks of coughing were. "Even as an adult, I found it compulsive." It felt like she had pulled muscles along her ribs, she says. But it was much worse for her daughter, who had asthma and was prone to illness. The five-year-old coughed for six months, making the characteristic whoop sound – which the disease is named after – when she gasped for breath. On one occasion when they were racing to the hospital, Lautenbach had to pull over the car every 10 minutes to give her daughter her inhaler and stop her from turning blue.
Thankfully Lautenbach's daughter survived that bout of whooping cough, as well as a later one as a teenager. The vaccine may well have saved her life. But it wasn't perfect, Lautenbach says she "didn’t realise until much later that the whooping cough one actually became less and less effective" over time.
Two generations of vaccines
Whooping cough is a highly contagious respiratory disease spread by the bacteria Bordetella pertussis (pertussis is another name for the illness). Pertussis, which typically resurges cyclically, is currently on the rise in many countries, after a quiet period during the Covid-19 pandemic. In the European Economic Area, more cases were reported between January and March 2024 than during all of 2023. In many countries, the number of pregnant women being vaccinated against pertussis has been declining. In the UK, 58.6% of pregnant women received the vaccine between 2023 and 2024, compared to 70.5% between 2019 and 2020.
Pertussis was part of the first-ever combination vaccine, DTP, which was first released in 1948 and is still in use today – it covers diphtheria, tetanus and pertussis. There are now several other options for combination vaccines including pertussis, most recently a six-in-one vaccine. Vaccines have made a tremendous difference to the severity of the illness. Before vaccination, on average, 10% of children with whooping cough died from it. Both infections and deaths dropped rapidly with the advent of vaccines. Whooping cough remains one of the most common causes of death that could have been prevented with vaccines. Vaccine effectiveness at preventing the disease typically ranges between 79% and 84%, with about 91% effectiveness in preventing hospitalisation.
 Getty Images
Getty ImagesDaniela Hozbor, a bacterial vaccine researcher at the Institute of Biology and Molecular Biology at La Plata National University, Argentina (IBBM UNLP-CONICET), explains just how easily pertussis spreads: if there's one infected person in a room, within an hour roughly 90% of susceptible people there may contract the disease. That's why it's so important to prevent pertussis with vaccination rather than simply relying on antibiotics afterward, which won't stop the contagion, Hozbor says. She is so passionate about communicating the importance of vaccination that she includes a reminder and a link to vaccination schedules in her email signature.
The world essentially has a two-tier system for pertussis vaccines. The first-generation whole-cell vaccines can have more serious effects like seizure, but are more effective and cheaper to produce. These whole-cell vaccines are used in many low and middle-income countries.
Second-generation acellular vaccines are administered in wealthier countries. These are safer but are based on just a handful of antigens – substances which can elicit an immune response – unlike the hundreds or thousands of antigens involved in whole-cell vaccines, explains Camille Locht, the research director of the French National Institute of Health and Medical Research (Inserm).
Locht has worked on multiple generations of whooping cough vaccines. As a junior scientist at a pharmaceutical company in the 1980s, researching acellular pertussis vaccines, he was convinced that including a toxin produced by the bacteria would help generate a potent immune response, he says. However, the acellular vaccines developed involved inactivating the toxin chemically, which he speculates might have destroyed some protective portions of the toxin.
When Locht left pharma for academia, he had a niggling feeling that the story of pertussis wasn't finished. Indeed, "what we didn't know at the time was that the vaccine didn't prevent infection," though it was very effective at preventing disease and reducing mortality from whooping cough.
 Getty Images
Getty ImagesYears later, heading up a lab at the Institut Pasteur de Lille, Locht went back to the drawing board on vaccines containing live, though weakened, pertussis organisms.
Third generation vaccines
New whooping cough vaccines are needed for several reasons. One is that the acellular vaccines, while still effective, are becoming slightly less so. A key reason is that the bacterial strains are evolving.
The ages of people contracting this infection are changing as well. Previously, it was mainly infants with incomplete vaccination who were developing whooping cough. It is still the case that deaths from whooping cough are mostly of children in this group. But now in countries including Denmark and Slovenia, the highest proportion of cases is in young people aged 10 to 19, when protection from an acellular vaccine has waned considerably.
"The problem with the acellular vaccine is that immunity is short-lived, much shorter-lived than with whole-cell vaccines," Locht says. A review of studies found that the effectiveness of acellular vaccines in 0- to 10-year-olds reduced from 98% in the first year to 81% five years after vaccination; and among 11- to 20-year-olds, it dropped from 72% in the first year to 42% four years post-vaccination.
Simply increasing the frequency of booster shots isn't workable, Locht says. For one thing, immunity to whooping cough reduces with further jabs, Locht says. In addition, people may tend to miss out on later doses, Hozbor notes. She says that in Argentina, a mother or a healthcare worker might need seven or more pertussis vaccine doses in a lifetime. (Argentina uses a whole-cell vaccine for the early childhood series, and an acellular vaccine for the boosters, as the risk of adverse effects increases with repeated whole-cell boosters.)
The third-generation vaccine that Locht is working on now mimics infection through weakened Bordetella pertussis bacteria. It's the furthest along of all the next-generation pertussis vaccines. Locht's employers sold the BPZE1 vaccine to ILiAD Biotechnologies, a small US pharmaceutical company, in 2013. Locht is also a scientific advisor to ILiAD, which he says aims to begin phase 3 clinical trials of the BPZE1 vaccine in 2025, to ensure that it is safe and effective in all age groups. Apart from minor side effects like a runny nose, Locht says, "we have not seen any vaccine-related adverse effects" in humans or non-humans. Distribution could start as early as 2026 or 2027, according to Locht.
There are some challenges to advancing the research. One is that for ethical reasons, a vaccine containing live bacteria cannot be tested immediately on young children. Locht has experienced firsthand the importance of nuance when discussing vaccine testing, finding himself embroiled in controversy after he appeared to agree with comments by another doctor in a TV during the Covid-19 pandemic. This led to accusations of racism, which Locht has denied, saying the discussion had been wrongly interpreted , and insisting his assent was to a more general point about the need for widespread testing of vaccines. The other doctor apologised, saying he had expressed himself "clumsily".
Importantly, the BPZE1 vaccine looks likely to be much longer-lasting than existing vaccines. It induces immunity markers not just in the blood, like acellular vaccines, but also in the nasal mucosa. This location is important. Kingston Mills, a professor of experimental immunology at Trinity College Dublin, believes that "what's clear from all the preclinical work is that nasally delivered vaccines are going to be the vaccines of the future for pertussis". He explains that existing injection-based vaccines generally "don't generate the responses in the nasal tissue and the lungs where the infection occurs. Whereas if you give the vaccine into the nose, it's much better at generating what we call the mucosal immune responses in the nasal cavity and the lungs". Mills' lab is also working on a nasal vaccine, not yet tested in humans, which kills the bacteria but makes it good at stimulating immune responses. "Nasal vaccines generate very good memory," he says.
 Getty Images
Getty ImagesMeanwhile, Hozbor's team is developing vaccines that could be delivered either through the nose or the muscle, focussing on outer-membrane vesicles derived from Bordetella pertussis. These spherical buds are naturally produced by them and have similar components and structure to the bacteria itself. When incorporated into vaccines, they can help to induce immunity. Outer-membrane vesicles of Bordetella pertussis are stable and stay in longer contact with immune cells, resulting in a stronger immune response and fewer adverse effects compared to whole-cell vaccines. Hozbor hopes that human trials will eventually show similarly positive results to the animal studies, but this will require time and funding.
Another versatile aspect of outer-membrane vesicles is that they could form the core of a vaccine themselves, or be added to other vaccines as adjuvants (substances which can enhance an immune response). Mills holds a patent on a different type of novel adjuvant; modifying such adjuvants may make vaccines better at generating important memory T cells. It's not yet clear how long immunity to pertussis would last in humans with these and other next-generation vaccines, but Locht hopes it could remain potent for decades
The limits and benefits of new vaccines
An important question is how acceptable new vaccines would be to the public. Parents may be more comfortable with vaccines given to their children as nasal sprays, as BPZE1 would be, rather than through injection, as the existing pertussis vaccines are. But this won't fully solve the issue of vaccine hesitancy. Hozbor stresses that more vaccine confidence is required overall, noting that since pertussis is so contagious, high vaccination of the population is needed to prevent outbreaks – ideally at least 90% or 95%.
Cost is another barrier to expansion of pertussis vaccination currently. In Malaysia, for instance, pertussis vaccination is only available privately. Locht hopes that the BPZE1 vaccine will be cheaper to make than the existing options. "You just grow the organism, harvest it and then use it," he says of the BPZE1 vaccine, while acknowledging that freeze-drying the substance may be the most expensive step.
However, vaccine affordability is much more complex than how cheaply they can be produced. It's not clear if pharmaceutical companies will be eager to replace a vaccine that involves multiple booster shots with an alternative that requires just one or two doses. In general, "pharmaceutical companies like drugs that they have to repeatedly give to patients or vaccines they have to repeatedly give to individuals," Mills notes. "But that's not what we need." Another consideration is whether to deliver next-generation pertussis vaccines on their own, or keep them as part of a combined childhood vaccine.
Overall, health experts emphasise that the current pertussis vaccines are safe and effective, and that vaccination is important to prevent severe disease.
Still, the vaccines can be improved. "Long-lasting vaccination would be amazing," says Lautenbach, whose family has experienced the long haul of whooping cough. If this had existed when her daughter was born, "I would have got it for her without hesitation".
--
If you liked this story, sign up for The Essential List newsletter – a handpicked selection of features, videos and can't-miss news, delivered to your inbox twice a week.
