How Covid-19's symptoms have changed with each new variant
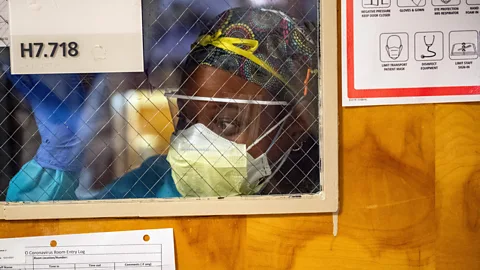 Getty Images
Getty ImagesWith a new variant of the Sars-CoV-2 virus causing a spike in cases, it is demonstrating just how much the disease has changed since the pandemic began – and what happened to "Covid toe".
"For almost four years, I've managed to dodge Covid-19," TV broadcaster Mehdi Hasan tweeted a fortnight ago. "But it finally got me. At the end of 2023."
Hasan added that his symptoms were thankfully mild, but he is just one of many people reporting their first ever positive test for the virus responsible for the pandemic, Sars-CoV-2, four years on from when it first began spreading around the world.
What are the symptoms of JN.1 and KP.2
The version of the Covid-19 virus behind the latest spike in infections shares many of the same symptoms as earlier variants of Sars-CoV-2 : a sore throat, fatigue, headache and a cough.
Differences in the symptoms often depend on a person's underlying health and their immune system. But some clinicians are reporting among the most common first signs of an infection by JN.1 are diarrhoea or a headache. Fewer patients are losing their sense of smell with variants closely-related to Omicron, of which JN.1 is a subvariant.
Another Omicron subvariant, KP.2 shares many genetic features with JN.1, but shows two distinctive mutations in its spike protein, leading to the nickname "FLiRT" as a way of describing specific amino acid changes. Although KP.2 has a higher reproductive number than JN.1, suggesting it is more transmissible, the virus itself has been found to be up to 10 times less infectious. It's symptoms are said to be similar to those experienced with other Omnicron variants.
Covid-19 cases are starting to rise again as a result of the KP.2 Covid subvariant, which was first reported on 2 January but started to become the dominant version of the virus in many countries in May 2024. By 13 May 2024, it accounted for 28% of cases in the US. It follows a rise in cases earlier in the year due to the JN.1 Covid subvariant, which appeared last September in France. This subvariant accounted for around 60% of new infections in early January, according to a data tracker from the US Centers for Disease Control and Prevention (CDC).
At the same time, data from both the CDC and the UK Health Security Agency shows that hospitalisations and deaths from Covid-19 are markedly lower compared to May 2023. Primary care physicians say they are finding it virtually impossible to distinguish Covid-19 symptoms from influenza without the help of a PCR test.
"When Covid first came, it was characterised by these very odd, vague symptoms – from brain fog, feeling exhausted, and losing taste and smell," says Ziad Tukmachi, a GP at Chartfield Surgery in south-west London, UK. "Now I feel it's mutated to more similar symptoms to the flu, where it's very difficult clinically to distinguish between the two."
While this might all suggest that the virus is evolving to become progressively less pathogenic, epidemiologists believe that the reality of the situation is more nuanced.
"The virus isn't necessarily less pathogenic," says Greg Towers, professor of molecular virology at University College London, UK. "Rather, it's infecting a population that are less inclined to become sick, because they've seen Sars-CoV-2 before, and they're better at regulating [their] immune response against it."
 Getty Images
Getty ImagesNow, in 2024, this is determined by a much more complex cocktail of factors, including how many times that person has already been infected by the virus, their vaccination status, and whether their vaccination-induced immunity might be on the wane.
As a result, Denis Nash, an epidemiologist at the City University of New York, US, says that people now experiencing Covid-19 for the very first time are at greater risk, especially if it has been a while since their last booster vaccine.
"There are still people who have somehow managed to remain completely Covid-näive," says Nash. "If they are unvaccinated or under vaccinated, they stand to have the highest risk of severe and protracted symptoms."
Still, Sars-CoV-2 is also constantly mutating, something which is also subtly shifting how it attempts to invade the human body. The JN.1 variant has an elevated ability to evade the immune system, for example, compared to other Omicron sub-variants. But this is also altering the way it affects the human body.
In 2023, researchers at Virginia Commonwealth University's School of Medicine reported that people now being infected with Omicron-related subvariants are just 6-7% as likely to lose their sense of smell or taste, compared to infections by the virus in the early stages of the Covid-19 pandemic.
Instead, some clinicians such as David Strain, associate professor of cardiometabolic health at the University of Exeter, UK, told the BBC that his patients are more likely to present either with diarrhoea or a headache having been infected with JN.1 or the EG.5 variants.
"There has been a huge shift in viral tropism, meaning which cells get infected," says Towers. "And that's governed by the sequence of the spike protein. Almost everybody in the world has been infected or vaccinated, so the virus is under huge pressure to escape those immune responses to continue to transmit, so the spike protein has evolved a lot. This leads to it infecting different cells to gain entry, which is why people aren't losing their smell or taste anymore."
Researchers are still trying to figure out whether some more subtle, internal consequences of Sars-CoV-2 infection varies between variants of the virus or whether any differences are more driven by the waning of previous vaccine-induced protection. One of the ongoing concerns remains the virus' ability to cause damage to blood vessels and internal organs through the creation of micro clots, with the kidney – an organ which is constructed of approximately one million tiny blood vessels called capillaries – seemingly particularly vulnerable based on the patients Strain has seen.
"These are just observations but we're seeing more microvascular complications and a step change in the kidney function with the new JN.1 variant that does appear to be worse than the past couple of variants," says Strain. "But it's difficult to say whether it's the variant, or the fact it's 18 months to two years now since a lot of people last received a vaccine."
 Getty Images
Getty ImagesWith some emerging evidence hinting that micro clots might be a cause of Long Covid – a study in August 2023 even suggested that they could contribute to the cognitive problems experienced by many Long Covid patients – researchers are now concerned that we might go on to see a further spike in chronic cases. However, it would be hard to distinguish whether this is a consequence of the new variant or declining population immunity.
"Studies from the March-summer 2020 period show that the risk of Long Covid from any case, was about 10%," says Danny Altmann, professor of immunology at Imperial College London. "Now we have far more infections, and the risk of Long Covid looks to have fallen, not because of a milder variant but because of a degree of protection from vaccine doses. A paper in the BMJ on a national cohort in Sweden shows protection goes up with each additional dose."
This all indicates the ongoing importance for all age groups of remaining up to date with vaccine boosters, but while politicians have long been keen to move on from Covid, Strain says it is vital to keep monitoring how different variants continue to infect us.
"Symptoms do seem to change from one variant to another," he says. "We've had periods where the earliest symptom is headache, and others where it's more gastrointestinal. We all to go back to life as normal, but the reality is, Covid isn't going anywhere."
--
Whatever happened to "Covid toe"?
In the early months of the Covid-19 pandemic, reports of an unusual and baffling symptom of the disease began to emerge – patients were developing painful or intolerably itchy lesions on their feet and hands. These chilblain-like swelling and reddening of the skin became commonly known as "Covid toe".
Doctors and scientists were puzzled – how did a respiratory virus cause such a strange symptom in the body's extremities?
Tests on samples taken from people with Covid toe have failed to find the presence of the virus responsible for Covid-19, Sars-CoV-2, in the chilblains, suggesting the virus itself is not directly responsible. Instead, a number of hypotheses have been put forward, including that it could be the result of an excessive response by part of the immune system that produces a protein called interferon IFN-1, which helps the immune system target cells infected by viruses.
Others have suggested that it may not be something specific to Covid-19 at all, and rather just a response that occurs in people who are prone to chilblains anyway.
Another theory was that lockdown rules meant more people were just not wearing adequate footwear around their homes and too much time sitting still.
Curiously, as the virus has evolved and lockdowns have lifted, so too has the apparent occurrence of these cutaneous problems. Research by scientists at King College London, UK, who studied the reported symptoms of more than 348,000 people who logged their Covid symptoms via a mobile app, has revealed that Covid toe and related skin complaints have decreased in more recent waves of the Sars-CoV-2 virus.
They were reported by 11% of people during the wave caused by the Omicron variant, compared to 17% in the Delta variant wave, where symptoms also tended to last longer.
* This article was originally published on 12 January 2024. It was updated on 13 May 2024 to include details about the Omicron subvariant KP.2.
--
If you liked this story, sign up for The Essential List newsletter – a handpicked selection of features, videos and can't-miss news, delivered to your inbox twice a week.