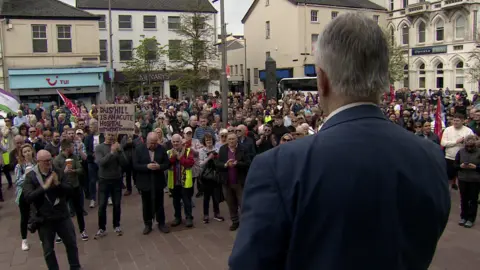
Daisy Hill Hospital's inpatient care 'at risk' in general medicine
 Pacemaker
PacemakerA shortage of consultants at Daisy Hill Hospital in Newry means delivering inpatient care in general medicine is at risk.
The Southern Health Trust said it was working with other trusts in Northern Ireland and the Department of Health "to help us through this situation".
It has also emerged that the hospital's stroke service is being withdrawn from 09:00 BST on 31 May.
That is because the hospital's one remaining specialist is leaving.
The trust said recruiting and retaining medical staff has been a major issue in the hospital in recent years.
"The pressures have now escalated with increasing reliance on medical locum cover and a number of consultant medical staff ending their tenure at the hospital," it added.
"These challenges are putting services at the hospital - such as respiratory and gastrointestinal (GI) inpatient medical provision - at risk.
"Every avenue is being pursued to protect services."
Southern Trust chief executive Dr Maria O'Kane told BBC's Evening Extra programme that in the last year "nine consultants have left and six of those left during the last three to six months".
With only one such medical consultant remaining, the trust has said it cannot staff rotas to ensure all services are delivered safely.
According to sources, senior management told a trust board meeting on Thursday it would take at least six months to stabilise the system, but action needed to be taken in advance of the summer holidays.
Medical consultants diagnose, admit and treat patients who may come into hospital via the emergency department (ED).
Their specialities include cardiovascular and respiratory disease, as well as gastrointestinal disease.
Without that expertise, a hospital is unable to function at its full capacity.
In future, people who become ill, including those who suffer a stroke, may have to travel to Craigavon, Ulster, or Royal Victoria Hospitals, or to a hospital in the Republic of Ireland.
It is understood senior staff plan to have talks with Our Lady of Lourdes Hospital in Drogheda.
Stroke patients to Craigavon
Craigavon Area Hospital, which is about 30 minutes drive from Daisy Hill, is likely to inherit most of the overflow.
The trust said that as there are "insufficient substantive stroke consultants at Daisy Hill", the decision had been taken "on patient safety grounds to again divert all acute stroke patients to Craigavon Area Hospital".
 Getty Images
Getty ImagesIt said this would come into effect from 09:00 on 31 May and that the same measure was taken in February "due to unforeseen staffing issues".
Craigavon Area Hospital often reports delays in its own emergency department.
In February, the Southern Health Trust announced the relocation of emergency general surgery from Daisy Hill to Craigavon.
Previously the trust had described that move as "interim" and due to ongoing recruitment challenges.
In October, the then health minister, Robin Swann announced that Daisy Hill Hospital was to become an elective overnight stay centre.
At the time, he said centres were being established as part of a reorganisation of surgery services.
Several clinicians and the public voiced concern about the future of the hospital.
Those consultants who have recently left Daisy Hill Hospital have retired, resigned, moved to another hospital in Northern Ireland or moved to the Republic of Ireland.
The trust, however, has insisted that general emergency surgery, the emergency department and maternity services were all currently safe.
 Pacemaker
PacemakerThe trust has said it plans to increase its acute care at home service.
That means patients who are normally admitted to hospital will be treated by clinicians at home instead.
Dr Tom Black, chairman of the British Medical Association (BMA) in Northern Ireland, said the announcement that some services are being withdrawn from Daisy Hill Hospital is "extremely worrying".
"Acute medical services at the hospital look increasingly precarious," he said.
"Transformation due to service collapse benefits neither patients nor doctors and destabilises services for patients.
"There will be a knock-on effect on services in Craigavon Hospital and any further attrition would impact GP services in the area as well, thus putting unacceptable pressure on different parts of the health service."
'Significant problem'
Dr Donal Duffin, was a consultant physician at Daisy Hill Hospital for a number of years, and is a member of the Daisy Hill Futures Group.
He said there had been a "significant problem" with the retention of senior staff at the Daisy Hill site and that the hospital was a critical part of the healthcare system in Northern Ireland.
"At the moment the remaining staff are pulling out all the stops, keeping things going as far as they can, but this is not a sustainable situation without a dramatic intervention by the trust, but I don't think that's enough, I think it has to involve the trust, the Department of Health and the politicians," he told BBC News NI.

Dr O'Kane told the trust's monthly board meeting that the shortage of consultants, difficulties recruiting specialist grade and junior doctors and the "serious over-reliance" on locum doctors "are matters of great concern in meeting the demand for acute inpatient medicine and providing stable medical staffing cover in our medical wards".
"This situation is certainly not unique to Daisy Hill Hospital," she said.
"The shortage of medical staff is extremely challenging in Northern Ireland, and indeed further afield."
She added that the trust continued to pursue every viable option to minimise the impact of this situation and stabilise its workforce.
Ms O'Kane said a meeting would take place next week involving all trusts to "seek support to address these challenges".
She said it needed to be recognised that medical staffing is "already stretched across Craigavon Area and other NI hospitals, so any support is likely to be limited".
"Our initial focus will be to stabilise staffing for the summer months in anticipation of a more permanent solution," she said.
"Ensuring patient safety and supporting our staff will be absolute priorities.
"We are very proud of the care provided by our medical staff, who have been working in very difficult circumstances."
Waiting lists
Separately, the number of people on hospital waiting lists in Northern Ireland has been described as "entirely unacceptable" by the Department of Health's permanent secretary Peter May.
The latest figures show that in the first quarter this year 401,201 people were waiting for their first outpatient appointment with a consultant.
That is 27,174 more than at the same time last year.
The statistics also show that 81% of patients were waiting more than nine weeks for a first consultant-led outpatient appointment.
One of the department's targets was that by March this year at least 50% of patients should wait no longer than nine weeks for this.
However, there has been some progress.
The number of inpatient and day case admissions waiting more than 13 weeks to be admitted for treatment was down, from 102,164 at the same time last year to 94,305 at the end of March.
The Northern Ireland director of the Royal College of Surgeons (RCS), Prof Mark Taylor expressed "grave concern" at the figures.
"The waiting time figures come on the back of a hammer blow to elective recovery this week by the Department of Health after it revealed plans to axe £34m from its waiting lists initiative programme due to huge budget pressures," he said.
