Sheffield maternity services rated inadequate by inspectors
 Geograph
GeographMothers and babies are being left at risk by failings at one of England's largest hospital trusts, a report says.
The health watchdog found Sheffield Teaching Hospitals lacked enough properly qualified staff to keep women and infants "safe from avoidable harm".
Despite warning trust chiefs last March, inspectors found maternity services had either failed to improve or "deteriorated further".
Trust chief Kirsten Major promised to make improvements.
The unannounced Care Quality Commission' (CQC) visit last October followed an inspection six months earlier that identified serious patient safety concerns and branded maternity services "inadequate".
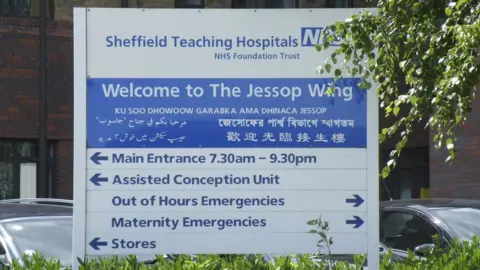
It found the Jessop Wing unit, previously rated "outstanding", did not provide "the standard of care women should be able to expect".
The subsequent reinspection found "there was little or no improvement to the quality of care patients received... in some areas the service had deteriorated further".
Inspectors found problems with cardiotocography (CTG) - used to measure a baby's heart rate - including poor documentation which fell short of national guidelines.
It comes as a similar concern was raised in a review of Shrewsbury and Telford NHS trust - the UK's biggest maternity scandal which saw more than 200 baby deaths.
In respect of Sheffield's maternity services, the most recent inspection also found:
- There were not enough midwifery and medical staff with the "right qualifications, skills and training to keep women and babies safe from avoidable harm and to provide the right care and treatment"
- "Significant concerns about the assessment of patients in the labour ward assessment unit, maternity staffing and delays in induction of labour"
- Foetal monitoring - previously highlighted as a concern by inspectors - "continued to lack urgency and pace in implementing actions and recommendations".
- Pain relief in labour was not always given in a timely way nor were assessments always regular
- "Staff did not always treat women with compassion and kindness, respect their privacy and dignity, or take account of their individual needs"
- Staff reported difficulties summoning assistance when a woman's health deteriorated
- Key information was not always included at shift changes and handovers
The CQC said analysis of data from April to October 2021 showed a "total of 35 patient safety incidents had been raised due to lack of suitably trained/skilled staff".
Staff also told the report authors about "two further serious incidents" that could not be found on the National Reporting and Learning System used to record such events.
This meant they could not be assured that all such incidents were logged and acted upon, the report said.
The CQC concluded: "We were not assured that leaders had the skills and abilities to run the service. We were concerned that leaders within the service were not effective in implementing meaningful changes that improved safety."
 Getty Images
Getty ImagesFurther concerns and the need for significant improvements were found across the wider trust, with its overall rating downgraded from "good" to "requires improvement".
CQC deputy chief inspector for the north Ann Ford said she recognised the "enormous pressure" NHS services faced but the watchdog was concerned that the trust's "leadership team didn't always have oversight and weren't always managing the risks effectively".
"It was most disappointing that several areas which we have identified in the last 12 months as needing urgent improvement had still not been fully addressed," she said.
'Vicious circle'
Trust chief Ms Major said: "We are all devastated with the outcome of the inspection because there is not one person within the trust who does not want to do the right thing for our patients and has not worked hard to try and deliver that in exceptional circumstances.
"That is why we are taking it extremely seriously and I will be doing everything in my power to support our staff and make the improvements we need to deliver."
"We have already taken action that will help us improve, including recruiting over 500 new nurses who are now working on the wards, and there have been changes to our maternity services including investing in more midwives."
Discussing staffing shortages, Karl Norwood, operational manager for the Royal College of Nursing in Yorkshire and the Humber, said there were currently 5,000 nursing vacancies in Yorkshire.
"It's no wonder that trusts like Sheffield, that in the past have had an excellent record of care and delivery, just don't have enough staff," he said.
"We're almost in a vicious circle, where nursing staff who are working are stressed and overstretched because they're covering huge gaps in the rotas.
"They're simply burnt out so we're seeing high levels of nurses leaving the profession."

Follow BBC Yorkshire on Facebook, Twitter and Instagram. Send your story ideas to [email protected].
