Coronavirus: The London hospital hit by a 'tidal wave' of patients
 BBC
BBCAs the UK stared down the barrel of a coronavirus epidemic in early March, the biggest fear was that hospitals would be swamped and incapacitated by a tsunami of patients. It happened in Wuhan and northern Italy. The NHS largely pulled through, but there were still times hospitals became overwhelmed. One of those was when a London hospital became suddenly engulfed with victims.
On 19 March, night-shift staff at Northwick Park Hospital in north-west London awoke to discover their workplace was so overwhelmed with Covid patients that a critical incident had been declared.
"I saw it on the news and thought 'oh my goodness'," said consultant Tariq Husain.
"I'd had messages from colleagues during the day saying it was getting really busy, we needed extra help, we've got such a volume of patients.
"It was that realisation that everything we feared was becoming reality.
"It was shocking and almost unbelievable that it was happening."
 BBC
BBC
 BBC
BBCWatching and waiting
 Getty Images
Getty ImagesSix weeks earlier, at the end of January, Brexit was the only story in town. Coronavirus was still a mystery disease silently circulating in China.
Northwick Park, which specialises in tropical diseases, was soon asked by Public Health England to start screening people coming into the UK from Wuhan who were showing signs of coronavirus.
The hospital's location makes it easy to access from Heathrow Airport - similar protocols were used during the Ebola outbreak five years earlier.
 Suhail Patel
Suhail PatelBy mid-February, the extent of the global spread of coronavirus was impossible to ignore. In Italy, the number of cases crept up slowly at first and then rapidly accelerated - a textbook epidemic curve.
Northwick Park staff were watching the news from abroad closely.
"I love Italy and go to Italy several times a year - I had actually cancelled a holiday that we had booked for the end of March," head of facilities Yvonne Smith said.
"So taking a particular interest in that and seeing the pictures of the intensive care units there was quite sobering, and you knew you were going to have to prepare yourself for something like that."
 Suhail Patel
Suhail PatelYvonne, from Kent, looks after non-clinical roles within the hospital - security, cleaning, porters, patient transport and laundry workers all fall under her remit.
"It's been extremely challenging because it has been so new and you don't know what to expect. It was a challenge managing all those groups of staff I look after in terms of making them safe at work, but making them feel confident in the job roles that they had."
Battle plans were drawn up in case Northwick Park experienced a similar onslaught to the one in northern Italy.
A pod was placed outside the hospital and any patients showing symptoms of coronavirus were assessed there. A specialist from the infectious disease department would don full PPE and come to test them.
 Suhail Patel
Suhail Patel Steve Watkins
Steve WatkinsInside the hospital, training exercises and preparations were just as rigorous. Some day-to-day tasks had to be scaled back.
"We mapped out a patient coming in as a live scenario and how we would have to adapt," A&E nurse consultant John Ross said. "Then we just trained and trained and trained for a good 10 or 12 days. So everything we did had to change because of the threat coming in with Covid."
John, from Inverness, explained that initial precautions against the virus were focused on identifying those patients who had travelled from China, Iran or Italy.
"For us, it was changing every single day. Which part of the world they were from and how much risk they had. I think Italy was when we really had to focus and get even more prepared - we kept saying in our training sessions that it was not likely to happen, but let's get prepared."
 Getty Images
Getty ImagesJohn knew that if a coronavirus wave was destined for the capital, the boroughs served by Northwick Park - Harrow, Brent and Ealing - would be likely to be hit hard.
"We saw what happened in Italy," John recalled. "We know there is a very dense population here, we know the demographics, we know a lot of our patients have cardiac and respiratory problems - a lot of diabetes - so it was always at the back of our minds.
"You hope that it isn't going to happen but you have to be prepared for it."
All of their intense training was about be put to the test.
 BBC
BBC
 BBC
BBC'It hit us like a tonne of bricks'
 Suhail Patel
Suhail PatelOn 3 March, "wash your hands" was the mantra at the Downing Street briefing - although Prime Minister Boris Johnson explained he had been continuing to shake people's hands. It was on this day the government published a detailed coronavirus action plan.
Ten miles from Downing Street, a patient turned up at Northwick Park who had just returned to London from Iran.
"We knew Covid was coming," said Dr Rachel Tennent, who specialises in respiratory medicine. "It had been in the news since January and we were preparing around February.
"Then it hit us like a tonne of bricks. It hit us hard and fast - the epicentre of the outbreak in the UK."
 Suhail Patel
Suhail PatelWhen a further two patients tested positive for coronavirus, the hospital triggered a set of rapid changes.
Surgeons were obliged to give up space so patients could be assessed safely and the A&E department was divided up.
"I remember meeting up here on Sunday 8 March - how we are going to keep staff and patients safe?" Rachel said. "We decided to create different pathways, negative going to one area of the department and people with respiratory problems who might be positive to the other.
"We had to move a lot of wards and staff around - stuff that would usually take six months to a year happened in a week."
 Suhail Patel
Suhail PatelThe number of seriously ill patients being admitted to Northwick Park was increasing and, within days, staff found themselves dealing with a crisis.
"We had an exponential increase," Rachel said. "On Monday 9 March we opened our respiratory assessment area wards and within two days those wards were full.
"Then on the third day another ward was opened and then we started cohorting patients with respiratory problems in side rooms. By the end of that second week we were up to a full ward and then another one full."
 Suhail Patel
Suhail PatelCoronavirus was declared a global epidemic by the World Health Organisation on 11 March.
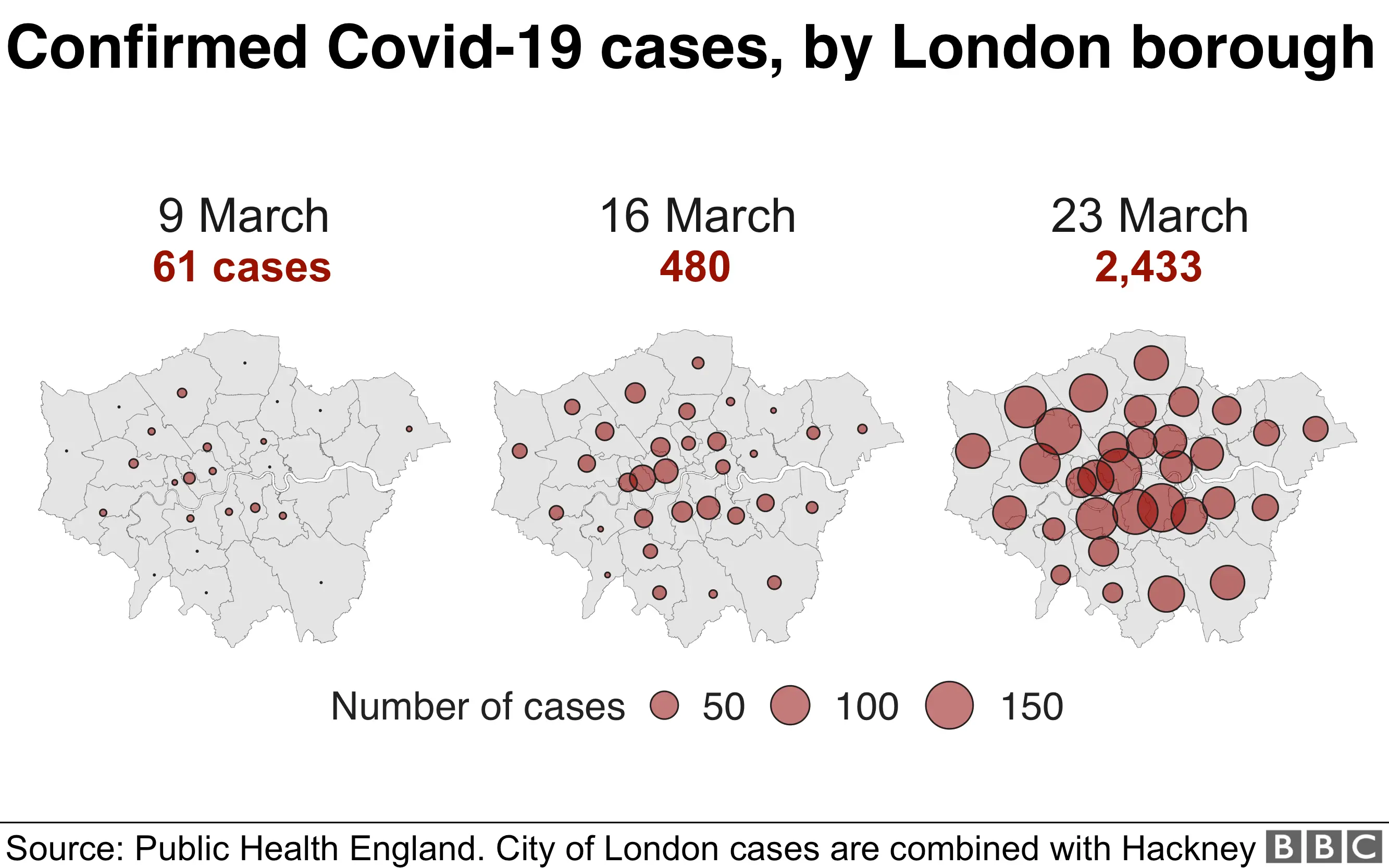
The virus was by now spreading across London, and Public Health England's modelling suggested cases were doubling in the capital every five days.
At Northwick Park, they were seeing the number of cases double every two days.
"It increased at a very, very rapid rate," Rachel explained, adding that new advice from China was that early intubation of patients was the way forward.
Risks are attached to every intubation as the procedure projects the virus into the air, further exposing staff.
 Suhail Patel
Suhail PatelAt this point, 44-year-old consultant Tariq Hussain had a tough conversation with his family after he was asked to take a senior role in Northwick Park's critical care response to Covid-19.
"It wasn't an easy call to make. You end up sacrificing a lot of things," Tariq said, although he knew that taking on the role was the right thing to do.
The gravity of the situation was by this stage clear, with confirmed infections in Harrow, Brent and nearby Ealing jumping from five to 112 in a week.
 BBC
BBC"We saw all kinds of patients - patients who have been admitted to ICU have been relatively fit and well, with a few diabetes, high blood pressure cases, but otherwise reasonably well," Tariq said.
"But certainly not just elderly; we had people in their 20s, 30s and upwards from there.
"There have been relatively few Caucasians and a high proportion of Asian patients, which is the cohort of people around here.
"Everyone had read the newspapers and seen the news about the scale of the pandemic, particularly in China.
"We never thought we'd quite reach the point of such a huge volume of patients requiring admission to intensive care."
 Suhail Patel
Suhail Patel"Patients would initially go into side rooms," head of facilities Yvonne Smith said. "Every time a Covid patient vacated that room it would need a full clean.
"So our normal terminal cleans will average 20 or 25 a day. At our absolute peak that went up to 96 terminal cleans a day."
Tariq described the surge of patients at this stage as a "tidal wave". It was about to crash down, as Northwick Park ran out of space for the sick.
 BBC
BBC
 BBC
BBC'We need help'
 Getty Images
Getty ImagesOn 19 March, the prime minister said it would take 12 weeks to turn the tide against coronavirus.
At the same time an executive meeting was being held at Northwick Park, where a critical incident was declared.
"We had a lot of patients and more coming in than we could match the demand of what we could actually do," head of nursing Trish Mukherjee said.
 Suhail Patel
Suhail PatelAs part of the critical incident protocol, patients were shuttled to other hospitals to alleviate the pressure.
"The whole point about the critical incident is for that help within the area," Dr Rachel Tennent said.
"You don't want people dying in a busy hospital when 30 miles up the road no-one has even got it, so the whole point is to share the access to ventilators."
 Suhail Patel
Suhail PatelNorthwick Park became the first UK hospital during the pandemic to declare such an incident - only Watford General has taken the same action, although Weston General also saw its resources pushed to the very limit.
Medical director Dr Martin Kuper was one of those involved in the decision to declare an emergency at Northwick Park.
"I think it was right for us to do so," he said. "We had an awful lot of patients and we needed some help here."
 Getty Images
Getty Images BBC
BBC
 BBC
BBCFrontline heartache
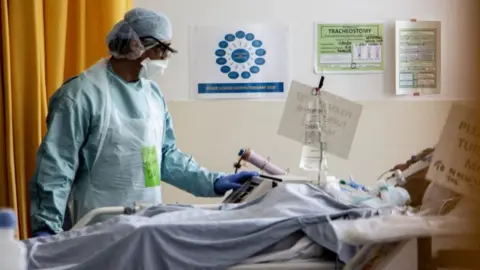
 Suhail Patel
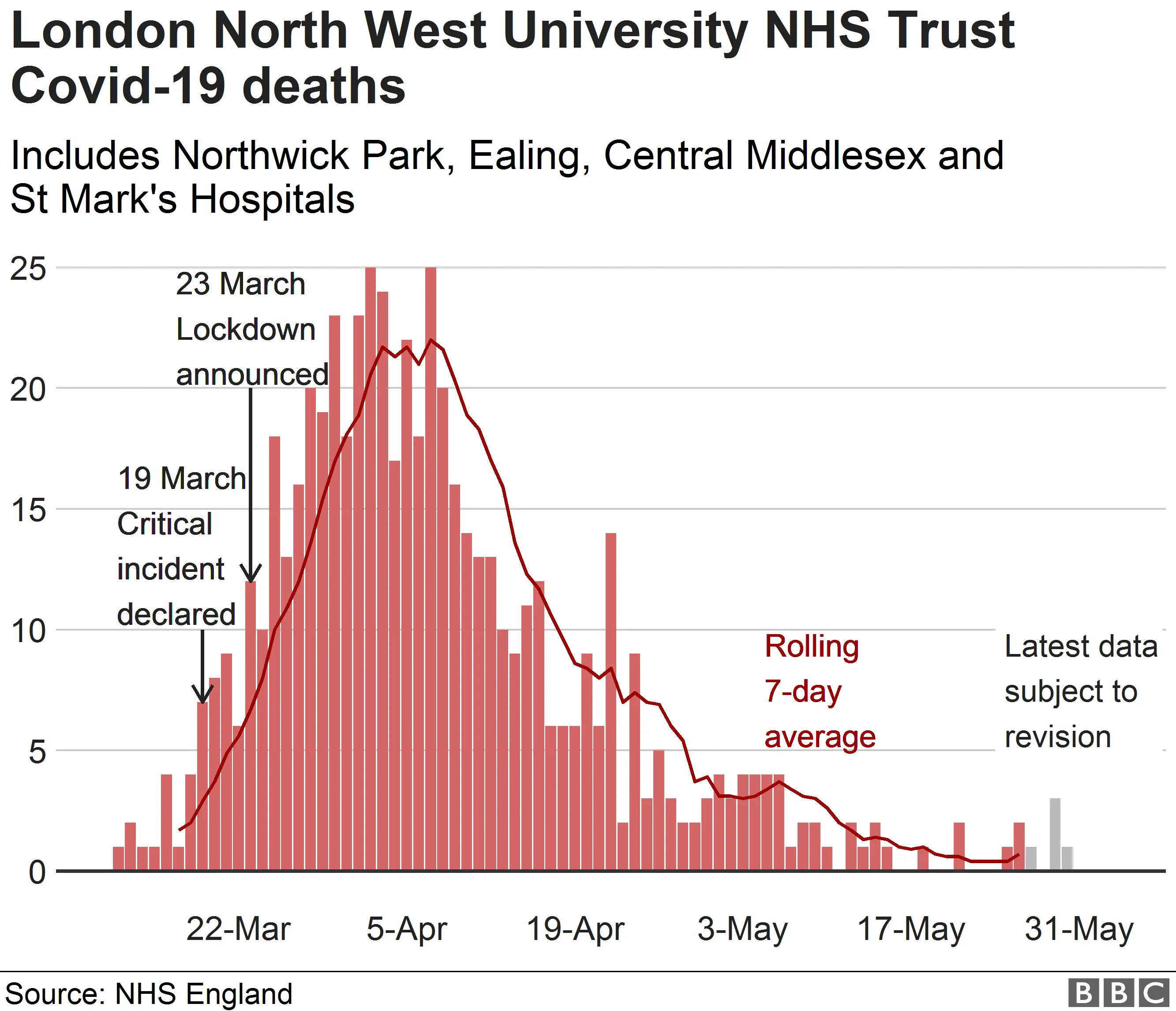
Suhail PatelTo stem the flow of coronavirus cases, the UK was put into lockdown on 23 March.
Restaurants, pubs and tourist hotspots emptied, while hospital beds and morgues continued to fill.
At the peak of the crisis at Northwick Park, 126 patients in the hospital's NHS trust area died with coronavirus in one week - every one of them with no family present.
"Yes, the deaths were going up," head of nursing Trish Mukherjee said, "but the most difficult part was that relatives weren't there and we had to stay with the patients and hold their hand and be there for their last moments - I think that was difficult in itself."
 BBC
BBCEmma Leahy, a nurse from Limerick, has the task of using a tablet computer to connect patients with loved ones at home.
"We continue to care throughout all different parts of their stays in intensive care," she said.
"Seeing a patient who we have cared for a month to be able to wake up and say 'thank you for looking after me', and seeing their children say 'can't wait to see you, Dad' - this is why we do this job."
 Suhail Patel
Suhail PatelOne of the people Emma has nursed is Jal Makai, a father of four from Northolt, who was taken to Northwick Park on 3 April after collapsing on the toilet.
In hospital, his condition worsened and within three days of being admitted he was hooked up to a ventilator. He spent a month on it.
His kidneys failed and he was unable to walk or hear out of one ear.
But Jal has survived.
 Suhail Patel
Suhail Patel"Without these guys at the NHS I'd be gone, very simple," he said. "At one point my wife thought that was it, I was gone."
He added: "When you do open your eyes there is someone here. Always - maybe even more than one. They are angels. They put themselves in harm's way - they should be getting paid more than footballers.
"If it wasn't for them I wouldn't see my kids again, very simple."
 Suhail Patel
Suhail PatelAt about the same time Jal was admitted, NHS veteran of 35 years Chris Bown took over as CEO of the London North West University Healthcare NHS Trust, which is responsible for Northwick Park.
"The striking thing for me is, having finished a job in the NHS as a CEO in mid-January, was that the NHS that I left in mid-January was not the NHS I returned to at the end of March," he said.
"It fundamentally had to shift and change to meet this devastating pandemic.
"I was really quite shocked to see the impact this was having but equally reassured that, despite the enormous pressures, the staff here in this trust were absolutely doing their utmost to manage very difficult circumstances with great compassion."
 Steve Watkins
Steve WatkinsEvery survival story during the pandemic has provided a much-needed morale boost for staff - and they have even had one of their own.
Nurse Alicia Borja spent a month in the hospital with coronavirus and was eventually applauded out of Northwick Park by the colleagues who helped save her.
Alicia is recovering at home but will be back to help care for others with the virus that almost killed her.
"We've had 900 discharges of Covid patients and that is amazing," Trish said. "It was lovely to see Alicia recover so well and to see her go home.
"I got to look after her, I got to speak with her, hold her hand and talk about normal things.
"Seeing her be applauded out was just an overwhelming joy."
 BBC
BBC
 BBC
BBCSecond wave fears
 Suhail Patel
Suhail PatelThere is now relative calm at Northwick Park. Covid patients are still coming in but at nowhere near the volume experienced a few weeks ago.
On the coronavirus ward, Emma Leahy takes a break from chatting with patients and families to reflect.
"The last few weeks have been emotional," she said.
"It has been a rollercoaster and it's made me realise we take things for granted - and it's something I won't be doing any more."
"Our work is being recognised," Emma added. "I never really knew my neighbours, they didn't really know me."
"They didn't know I was a nurse and the last few weeks I've gotten to see my neighbours and we've clapped for carers every Thursday together and it has just brought this sense of community and the feeling that we are all in this together."
 Suhail Patel
Suhail Patel"North-west London is where the wave crashed in Covid and we were the hardest hit first," medical director Martin Kupar said.
"The reasons for that, our boroughs, Brent, Ealing and Harrow, have a high rate of Covid.
"We don't know why that is - it is certainly a diverse and multi-ethnic area and then there is a lot of travel as well. There are also socio-economic reasons."
 Getty Images
Getty ImagesHe said that patient numbers did not double again at Northwick Park after the critical incident was declared. More than two months on, staff now fear a second wave.
"We were the place that was hit first but it would have carried on - the lockdown was essential. Nothing else can help you reduce the numbers," he said.
"It seems likely that there will be upstrokes of waves as the lockdown is eased... the rate of increase is likely to be slower than the first time round, which is when there were no restrictions on people.
"I don't think we've had a similar crisis in my lifetime in the NHS and I think the staff have been amazing."
Allow Google YouTube content?
Many staff are being encouraged to take time off.
"Of course we are on standby in case anything increases," CEO Chris Bown said. "But we are seeing that the numbers of admissions and deaths through Covid-19 have decreased substantially.
"Clearly, we are all learning a great deal from this and we always need to be prepared if there is going to be a second wave - which we really hope there isn't - but we are now making sure staff take as much annual leave and training as we are in a bit of a dip right now."
It's now almost three months since the first confirmed coronavirus patient was admitted to the hospital.
Even though the past few weeks have been traumatic, there is a sense of triumph in the unity, compassion and resilience shown by staff at Northwick Park.
Exhausted nurses, doctors, cleaners and porters are cautiously optimistic they have overcome the biggest challenge of their working lives - but remain wary of a return to the all-consuming fight against an invisible enemy.
 Wembley Stadium
Wembley StadiumAll images subject to copyright
