Health service pressures are dire and diabolical - O'Neill
 BBC
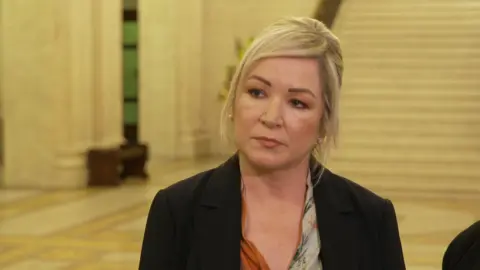
BBCPressures facing Northern Ireland's health service at the moment are "dire and diabolical," First Minister Michelle O'Neill has said.
She was speaking as MLAs, who officially returned to the assembly after winter recess, are facing calls to do more to alleviate the current situation.
During a motion on Ambulance waiting times, the Health Minister Mike Nesbitt told MLAs in Stormont, he accepted there was "an urgent need for reform".
It has been a challenging fortnight for emergency departments in Northern Ireland.
Last week the director of the Northern Ireland Ambulance Service (NIAS) said delays getting patients into emergency departments were leading to increased deaths.
The motion, called for by the Alliance Party, expressed the grave concern at the pressure facing the ambulance service.
'Public want to hear what we're going to do'
Addressing reporters, O'Neill said it was "dire" not just for patients waiting on a bed, but also for healthcare staff.
"We've work to do - one minister will not solve that, there needs to be a collective effort," she said.
"The public want to hear what we're going to do about it, we know what the challenges are and the issue of discharges into social care aren't there - that's what I want the executive to talk about."
Last week, Health Minister Mike Nesbitt announced flu vaccines, currently available for free to those aged 65 and over, would be extended to the 50-64 age group.
Nesbitt also said he plans to increase the wages for social care workers in a bid to "stabilise" the health system.
During the crisis last week, the Department of Health said longer-term solutions to the problems required sustained investment and reform.
 PA Media
PA MediaSpeaking at Stormont, Nesbitt claimed his goal was "to develop a better, more equitable, more effective and better integrated, urgent emergency care service".
He said the current pressures stem from an inadequate budget.
"If you're told the budget is entirely inadequate to meet the needs of the HSC service, and then vote for it, despite the warning, and then complain about the consequences of your decision, are you comfortable taking that position?"
He announced a number of steps his department would take to help with the quality of our health system.
He added: "It is essential we have sufficient capacity and that's why in the coming months I'll be commissioning an evidence-based emergency care capacity review."
This included taking action to increase ambulance service capacity.
Alliance MLA Stewart Dickson told the assembly that in England and Wales people who need to move from hospital into assisted help in the community have "to battle with local authorities".
He continued: "Here we have a joined up, allegedly, health and social care system. Yet that joined up bit has failed us."
DUP MLA Diane Dodds, who sits on the health committee, said today's problems represent failures which have a been made repeatedly in the past.
Meanwhile, SDLP MLA Colm McGrath, who also sits on the committee, said: "People are afraid that whenever they get to the point where they need an ambulance and they lift the phone... that there isn't immediately somebody at the other end that is able to come and help them."
How long are A&E waiting times?
A cold snap coupled with the winter flu surge were factors in the delays of the last two weeks.
At one point hundreds of people were waiting for more than 12 hours in Northern Ireland's nine emergency departments, with more than 1,000 waiting to be treated in total.
A lack of care in the community meant hospitals had difficulties discharging patients, leading to longer wait times to be admitted.
Two elderly patients were reported to have been in the Royal Victoria Hospital's emergency department for more than five days.
One nurse from the hospital said staff were treating "the most vulnerable elderly sick patients in an intolerable environment".
The vice-chair of the Royal College of Emergency Medicine in Northern Ireland said the issues in emergency departments were "at the worst we've ever been".
Dr Michael Perry added that a 12-hour wait for a bed was probably a "conservative estimate".

On Sunday, a consultant surgeon said that Northern Ireland's emergency departments have been in the midst of a "perfect storm" due to ongoing "immense pressure" and flu.
Prof Mark Taylor, from the Northern Ireland Confederation for Health and Social Care (NICON), said the lack of flow throughout hospitals was having serious consequences.
Prof Taylor also said that at 10:00 GMT on Saturday there were 532 people who were medically fit for discharge, across NI hospitals, but could not be discharged into the community.
