Asylum seekers need dedicated GP healthcare, Welsh doctor says
 PA
PARefugees and asylum seekers need dedicated GP services to get the health care they need, a doctor has said.
Dr Sophie Quinney, who has treated new arrivals in Cardiff, said language, transport and other barriers mean they struggle to use mainstream services.
She also claimed general practices were not geared to help disorientated and traumatised people.
The Welsh Government said it was investing in specialist mental health services which GPs could access.
Updated guidance published for consultation says refugees and asylum seekers "suffer disproportionately when compared with the general population" in relation to access to healthcare and outcomes.
Ministers want them to use mainstream NHS services, but admit "a model of care to facilitate and support integration, or to ensure public health issues are addressed, may initially be appropriate".
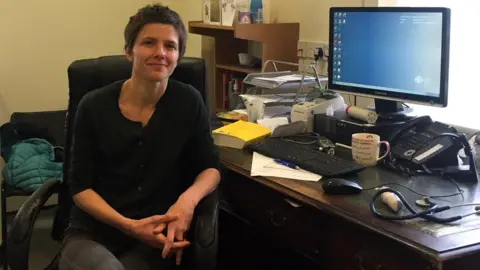
Dr Quinney, a locum GP who has worked at the Cardiff Health Access Practice (CHAP), said it was designed to respond to the needs of newly-arrived asylum seekers, with Iran, Afghanistan and Syria among the main countries of origin.
She said problems arose because they are encouraged to register with a general practice as soon as they are sent to Cardiff by the Home Office.
"They struggle to be understood, they don't understand how the appointments systems work, they find it very difficult to get to the appointment in time, they can't cope with the 10-minute appointment system because there's a language barrier," she said.
 cardiff health access practice
cardiff health access practiceDr Quinney, who also works in mainstream GP practices, said CHAP can offer refugees and asylum seekers longer and more flexible appointments, and more support for conditions such as post-traumatic stress disorder.
"Usually there's a delay in the onset of these symptoms - nightmares, flashbacks and extreme anxiety - of around three months after the initial trauma in their home country.
"It's compounded by social isolation - living in Cardiff and not being able to work makes these symptoms worse."
The role of CHAP has been expanded to include non-medical activities such as reflexology, birth partners and gym projects offered by volunteers.
Dr Quinney said these were not standard GP services, but claimed they were "critical" to helping asylum seekers cope on arrival.

Gym therapy
 Cardiff Health Access Practice
Cardiff Health Access PracticeEstelle Tije, 33, from Cameroon, had completed a master's degree in nursing in London when she heard her father had been killed during political turmoil in her home country.
She applied for asylum in November when her student visa expired and was sent by the Home Office to Cardiff.
Ms Tije paid tribute to Dr Quinney and the CHAP team for helping her cope with life in an unfamiliar city without resorting to pills and prescriptions.
"I went through a lot of stress - she really helped me by sending me to the gym," she said.
"I didn't want medication - I'm a nurse so I understand each medicine has a side effect.
"But through the gym I managed a coping mechanism to overcome that stress."

'Workload pressures'
The Welsh Government said GPs were able to refer to specialist mental health services, with £40,000 provided in 2017 specifically to train staff in trauma-focused care for refugees and asylum seekers.
A spokesman said: "Since we published our original guidance in 2009 we have seen significant changes as a result of increasing conflict in the middle and near east.
"Our latest draft guidance provides an update and will support healthcare professionals working with refugees and asylum seekers."
Dr Jane Fenton-May, vice-chairwoman of the Royal College of General Practitioners Wales, said: "All staff working in a practice should be aware of the cultural needs of any patient and accessible training and support could help improve that.
"How to best achieve this when GPs are facing severe workload pressures will need to be considered."