NHS Wales: Plan to cut waiting lists to a year by 2025
 Charlotte Camp
Charlotte Camp Patients have spoken of living in pain, waiting years for surgery, after a plan to cut NHS waiting times was published.
The Welsh government has promised no-one will wait longer than a year for planned treatment - in most specialities - by 2025.
Charlotte Camp said she had been left "screaming in pain" awaiting surgery for endometriosis.
The 28-year-old is one of tens of thousands of patients who have waited more than a year for surgery.
Latest figures show patients have been waiting more than a year for 168,521 procedures in Wales.
That figure was fewer than 7,000 two years ago, but waiting times have grown to record highs during the pandemic.
'Going private is not viable'
Ms Camp, from Neath, was diagnosed with endometriosis when she was 17, and in November 2020 was told it was on her bowel. She is now waiting for surgery to try and remove it.
"At the moment it's a six-and-a-half year waiting list," she said, adding she had looked at going private for the surgery but it would cost about £10,000.
"I'm crawling up the stairs screaming in pain and it's not something I want my family or four-year-old daughter to see and it scares me," she said.
She added: "I have looked at going private but it's extortionate and with a family and a house to run it's just not viable for us unfortunately."
A year for first appointment
Planned care, or elective care, covers all services where patients are referred on for extra services or treatments - be that outpatients, dental, optometry, mental health or surgery.
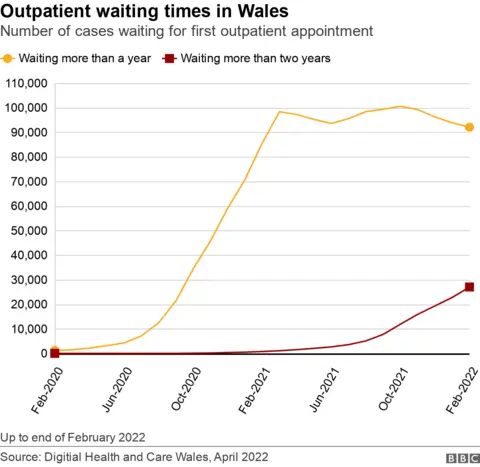
Under its recovery plan, the Welsh government has pledged that by the end of 2022 no one will wait longer than a year for their first outpatient appointment. Currently there are 92,130 in that position.
The number waiting more than two years for a first outpatient appointment has jumped from just four patients before the pandemic to 27,049 in February.
The plan also promises to increase the speed of diagnostic testing for therapies by spring 2024.
By 2026, it said 80% of patients will get a cancer diagnosis and treatment within 62 days - the current target of 75% has never been met and stands at 59.5%.
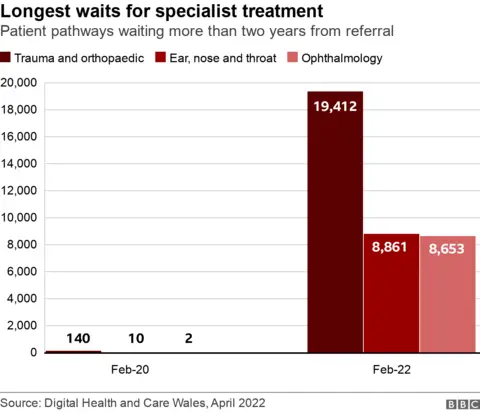
In trauma and orthopaedics, there are 19,412 patient pathways with waits of more than two years for treatment to start after referral.
This means more than a third of the people who are waiting more than nine months for their orthopaedic treatment to start are facing these longest waits.
'Concerns over orthopaedics'

Welsh health minister Eluned Morgan told Radio Wales Breakfast that she had "reservations" that targets could be met in orthopaedics.
She said a target had been set "and we will be working towards that".
"That is the only speciality where I do have some reservations," she said, adding: "That's the only area where I have my concerns."
She said there will be trauma and orthopaedic centres specifically for planned care, such as at the Royal Gwent Hospital.
She told a later briefing that while efforts would be made to make sure targets were reached orthopaedics was less predictable than some other areas, due to procedures being "knocked out" by emergency cases, and a lack of beds.
"What we're hoping to do is to develop high volume places that are what they call green lanes, where they are kept apart from accidents and emergencies, so that we can get our consultants actually doing the operations that they're very keen to do," she said.
As for other specialisms, those waiting more than two years for ear, nose and throat treatment to start have risen from 10 patients before the pandemic hit to 8,861 in February.
In ophthalmology, 8,653 have been waiting more than two years for treatment to start, compared to just two before the pandemic.

Jessica Ricketts, from Barry, has been waiting three years for a hysterectomy and said: "Every day there's some sort of pain".
Ms Ricketts has been struggling with pain caused by endometriosis despite six gynaecological surgeries over the past 10 years.
She told BBC Radio Wales Breakfast show she felt she and other women had been pushed to the bottom of the list, and she felt she had been forgotten.
Ms Ricketts said she was admitted to hospital two weeks ago because she was in so much pain, and she spends her life trying to manage the symptoms.
"My fear is that the endometriosis - because obviously I'm just waiting - is now in my diaphragm, and so I get pain on my left side," she said.
"With every day almost, which used to just be cyclical and now it's gone a lot worse," she said, adding that having hormonal treatments while waiting for surgery was impacting her mental health.
"It's trying to decide which is worse. Do you take the hormones to try and suppress the symptoms and then get the mental health symptoms or do you not to take the hormones and deal with pain?
"And for me, I find dealing with pain, a bit more manageable."
The recovery plan says in addition to almost 700,000 people on waiting lists, "it is also estimated that around 500,000 referrals have not been received in secondary care services over the last two years".
As a consequence, "we do not think that the waiting list will start to stabilise for the next nine to 12 months, perhaps longer".
In addition to increasing capacity, the plan also sets out promises to give better information to patients waiting, as well as support and a focus on "those with the greatest clinical need".
'Chronic shortage of staff'
Dr Hilary Williams, Royal College of Physicians regional adviser for south east Wales, said it left them with questions over delivery of the plan.
"We know that the chronic shortage of NHS staff is a very limiting factor to reducing the backlog, and there's simply no real detail on that," she said.
"How many doctors, nurses and allied health professionals will we need in the next five years, to actually meet some of these targets on diagnosis and treatment?
"There are some really good strategies out there. But we need to work much more closely together. We need detailed delivery plans: we need to know projected numbers of staff, how they're going to be funded, how they're going to be trained.
"If we work together, we can get there, but we need a much more collaborative approach from the Welsh government."
Under the new plans, an extra £60m will be given to health boards over the next four years, bringing the Covid recovery NHS budget to around £1bn.
The plan also sets a target of about a third (35%) of new appointments and half of follow-up appointments to take place virtually in future, freeing up clinicians' time.
But Welsh Conservatives have called the plans "unambitious", while Plaid Cymru called for focus on prevention.
 Digital Health and Care Wales
Digital Health and Care Wales

When you break down the number of people waiting a significant amount of time for an appointment, you get a sense of the scale of the challenge facing the NHS.
Because some of these numbers are eye-watering.
Even the shortest, arguably most straight forward target - a first outpatient appointment within a year - will take until the end of this year to meet and already impacts around 92,000 people.
By March next year there could still be some areas where people are waiting more than two years.
The minister has always said it will take the life of this Senedd term to tackle the backlog - these figures flesh that out, though will provide little comfort for those who have already faced long, painful waits.

- WOMEN OF WALES: Showcasing amazing Welsh female talent and stories
- PEOPLE THOUGHT OF AS BITS OF AN ALGORITHM: Life and death in the warehouse

