A&E units continue to struggle on waiting times
 Neighbours' photo
Neighbours' photoAccident and emergency departments in Welsh hospitals continued to struggle in October after recording the worst performance figures ever in September.
October's figures showed just 75.3% of patients were admitted, transferred or discharged within four hours in urgent care departments which include A&E - compared with the target of 95%.
September's figure was also 75.3%.
The Welsh Government said it had again provided an extra £30m to help prepare the system for winter.
There was some improvement in the number of patients facing the longest waits, with those waiting more than 12 hours decreasing slightly from 5,708 in September to 5,581 in October.
But performance on both four-hour waits and 12-hour waits was significantly worse than at the same time last year.
Ambulance response times
The figures also show a deterioration in ambulance response times to the most serious 999 calls over the course of the year.
In October 2018, an emergency vehicle arrived within eight minutes to 74.7% of "red" calls - those where a life could be immediately at risk.
Last month that figure had dropped to 66.3%, but was still above the target of 65%.
The Welsh Government said the ambulance service was having to deal with a 35% increase since 2015 in the number of the most serious red calls.
A spokesman said: "Last month was the busiest October on record for emergency departments in Wales and the ambulance service had the busiest month ever for the most serious 'red' calls...
"Despite this, the average waiting times in emergency departments have remained steady and the ambulance service exceeded its target for the 49th consecutive month. The number of delayed transfers of care also decreased in October."
He said they had provided the annual extra funding to health boards and councils earlier than usual in preparation for the anticipated increased pressure on the system over winter.
Accident and emergency performance across the UK
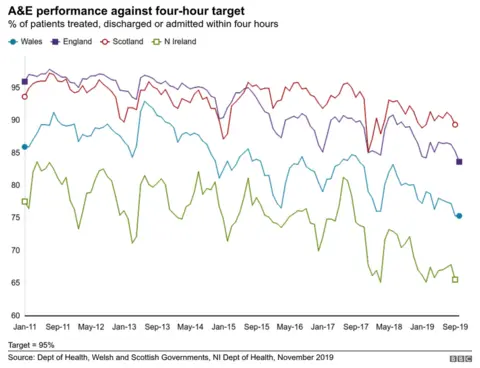
BBC analysis of the latest available statistics show all nations in the UK have seen a rise in the number of patients attending emergency units.
In Scotland though, the rise has been about a third of the increase in Northern Ireland and less than half the rise in England.
Wales is now beyond a million patients using A&E every year. The proportional rise between 2011 and 2019 was 13.5%.

The domino effect of waiting times

In late September, 67-year-old Geraint Morris fell and broke his hip outside his home in Pontardawe. An ambulance was called and passing workmen and neighbours covered him with jackets and erected a tarpaulin to shelter him from torrential rain. He could not be moved because of excruciating pain.
It took five hours for the ambulance to arrive.
"I was in pain - I didn't know what was going on," he said.
Despite the wait, he had nothing but praise for the medical staff who treated him and once in hospital he said it was "very good" but busy. He is now recovering well.
The Welsh Ambulance Service apologised, explaining it had been one of the busiest days in the previous 18 months. Ambulances had been snarled up at Morriston hospital because of waits in accident and emergency.
It is just one example of how problems in one part of the NHS can knock on to others.
 Neighbours' photo
Neighbours' photo
How is NHS Wales coping?
Dr Andrew Goodall, NHS Wales chief executive, said they had been working to prepare for the winter and get extra capacity into the system.
He said 2019 had been the busiest year on record on several measures including A&E, and ambulances, in particular the most urgent "red" calls.
"There are plans in place to be as prepared and as resilient as we can be through the winter but it will not take away that there will be some challenging periods for us, not least because we can look back at some of our recent experiences."

While the NHS has been focusing on prevention - such as expanding the flu vaccination programme and the Choose Well campaign aimed at directing patients to the most appropriate service - there are some pressures that are out of their hands.
"The impact of older people and their needs and their admissions over recent years, that is a trend... that is something that has built up over the last few years, and you do see that enhancing particularly through the winter months, where there'll be a high level of older people coming through the system," he said.
"We have seen some pressures around mental health... I hope that some of that is because there is a broader awareness in terms of accommodating patients with mental health needs.
"The strong drive for many of our pressures will be patients coming in with complex conditions and the age associated with those conditions."