Cwm Taf maternity: Mothers ignored and made to feel worthless
The full extent of the problems with maternity services at two hospitals in the south Wales valleys rings out when the voices of women and families are listened to.
"Overwhelmingly" mothers faced "distressing experiences and poor care", the review team found.
As one said: "I want having a baby to be a good experience. It's ruined it."
Women repeatedly stated they were not listened to and their concerns were not taken seriously or valued.
They spoke of being ignored or patronised while being cared for at the Royal Glamorgan Hospital in Llantrisant and Prince Charles Hospital in Merthyr Tydfil.
Often, their suspicions and concerns were found to have reflected a genuine problem that emerged later, but at the time they were dismissed when they tried to voice their concerns.
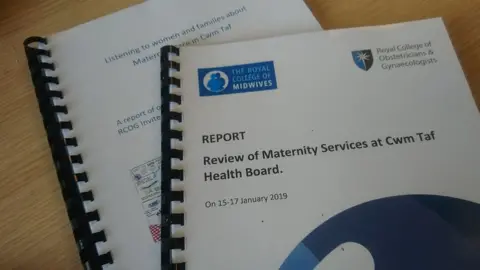
A major independent review has found Cwm Taf health board's maternity services were "under extreme pressure" and the health minister has ordered them be put into special measures.
It was prompted by 25 serious incidents, including eight stillbirths and four neonatal deaths, between January 2016 and last September.
The independent review team has released a separate, damning 78-page report, which shares the views of 140 family members, including mothers about their experiences at the hospitals.
Nearly two thirds of women questioned felt they had not had good quality care during their pregnancy.
The review said: "Many women had felt something was wrong with their baby or tried to convey the level of pain they were experiencing but they were ignored or patronised, and no action was taken, with tragic outcomes including stillbirth and neonatal death of their babies."
One woman said she felt worthless, adding: "I'm broken from the whole experience, the lack of care and compassion."
On the care itself, repeatedly the review team heard from mothers who did not always believe the right level of skills and expertise were available at the right time.
There was a failure to seek a second, more senior opinion, and to escalate concerns, especially with women with complex pregnancies.
One mother said: "He told me there was no point calling the consultant on a Sunday as no one would come."
Another said: "I never saw the same consultant. They didn't know me, and they didn't want to know me. I was pushed in and out of rooms with all sorts of people."
Mothers faced too many variables in the service offered - from the time of day they used it, to staffing levels and the communication skills of the staff they met.

The case of Sarah Handy
Sarah Handy's experience is highlighted in the report as illustrating a number of serious issues.
In pain, she was begging to see a doctor when she arrived in hospital in April 2017 and was left for nearly three hours without examination before being told it was constipation.
Ms Handy, 33, was sent back home to Merthyr Tydfil with laxatives and pain relief and that evening her baby Jennifer was delivered prematurely by her husband and mother-in-law.
Despite their efforts to give CPR to save her life, Jennifer died.
The review said it showed:
- Inadequate levels of expertise in managing high risk pregnancies
- Failure to listen to women and to understand the level of pain being experienced and reported
- Lack of response to "red flags" and failure to follow good practice and pathways of care
- Failure to call for a second, more senior, opinion
- Failure to support the woman after the tragic and traumatic loss of her baby.
Ms Handy said after the report came out: "Today it's been proven in black and white that we were right to highlight our concerns and push for further investigation into our Jennifer's death.
"We just wish that this report will now do what it promised and improve the quality of care so that no other family has to go the traumatic experience we went through."

On communication, although individual staff were spoken of as excellent, many women felt during their care this aspect was extremely poor.
When concerns were raised, there was a "significant dissatisfaction" with how they were dealt with, with dismissive attitudes.
Many women were not listened to or taken seriously, one saying she was "laughed at" when she expressed concern.
Other responses included: "I was never asked, never believed.
"If only they had asked the right questions.
"Most importantly, we were not listened to. By the time we were it was too late."
The review said women reported an "almost callous and brutal use of language" and disregard for feelings.
When one mother was concerned that she may be losing her baby she was told to "prepare for the worst - it could be a miscarriage" and then told to go home as "there wasn't a lot she could do."
Younger mothers in particular often felt their concerns were dismissed, which became an "emerging theme" for the review team.
There were failures to apologise, lack of access to notes and comprehensive investigations over concerns.
With high risk pregnancies, one woman interviewed believed that there was a lack of expertise and that "anything different from the norm, they didn't seem set up to deal with it".
Another described the antenatal clinic as being "like a cattle-market".
When babies were lost, "many women and families received no bereavement counselling or support and continue to experience emotional distress".
But staffing shortages were recognised.
 sturti/Getty Images
sturti/Getty ImagesOne mother talking about the demand on midwives and doctors in the Royal Glamorgan Hospital, said it was "no way a reflection on them".
"They would always spend as much time as possible with me but unfortunately when needs must I was left with some questions but again this was due to staff shortages," she said.
Another said: "There were so many jobs for one midwife to do and then people wonder why mistakes get made. They are human and are exhausted".
The review team said it was disappointing that lessons had not been learnt from a review of Furness General Hospital services four years ago.
Prof Jean White, chief nursing officer, said: "It should be a joyous occasion giving birth to a child. Many of the women who shared their stories had care well below the standards we expect and that's not right.
"I think over time there appears to be a culture that has developed rather than an open culture where people are encouraged to say what's gone wrong, there is a blame culture."
In the words of another parent: "Listen to women and families and believe what they tell you when they are in pain."
The review team concludes: "The strong message heard from women and families in Cwm Taf is that they don't want their experiences to happen to anyone else and the importance to them that the organisation learns from these experiences to ensure that improvement and change occurs."
Cwm Taf chief executive Allison Williams said she was deeply sorry, is taking the findings very seriously but recognised "significant work" was still needed.
"Some of the feedback we have received from patients is extremely distressing and their experience in our maternity service has been totally unacceptable," she added.

If you have been affected by stillbirth, the following organisations might be able to help:
