Coronavirus: Charities plead for restart to disrupted cancer services
 BBC
BBCCancer charities are calling for an urgent plan from the Scottish government to safely restart cancer services disrupted by Covid-19.
The coronavirus response has seen screening programmes paused, urgent referrals for diagnosis dropping sharply and surgery suspended for many cancer patients.
Specialists have voiced concerned about the long-term impact on survival.
Hospitals have had to change the way they deliver remaining services.
'They said I'd be done for'
The Western General Hospital in Edinburgh has managed to keep about 80-90% of non-surgical treatment going through the pandemic.
Patient Jean Greig was worried Covid-19 would adversely affect her treatment for the lung cancer that has spread to her liver.
She told the BBC: "The call came in February or March. They said about the coronavirus, and that with the cancer I've got I would be done for, and that I would need to consider maybe a DNR (Do not resuscitate order). So at that, I was shattered.
"My worry was that they wouldn't do the treatment. That was my greatest concern. I knew this thing was there and it was growing."
But her chemotherapy went ahead, after exploring the risks and treatment options with her oncologist. She is now on her third of four chemotherapy sessions - and things are looking positive.

"The oncologist has been brilliant. She says the chemo's working, and that the tumour that they saw on my liver is now half the size. So they'll now continue with the therapy in the hope that it will take it away altogether."
But she's still a bit uneasy about coming into the hospital.
"I still have a wee concern. They're telling me I'm in high risk, and I can't go out, I can't do this, but you can go to the hospital and sit with strangers. It's all a bit weird. They'll obviously do the best that they can to keep it at bay."
Hospital zones
In order to do this, the whole hospital has been zoned into Covid and non-Covid areas, including the Cancer Centre. More space has been created in waiting areas and clinics are mostly held remotely by video call.
Everyone who arrives through the front door gets screened for symptoms.

"We have a clear pathway should anything come up from that," says senior oncology charge nurse Jane Curran. "Yes we have patients that come in with symptoms, but they're managed pretty speedily. I think the system is working very well."
Doctors are also learning more about the particular risks for cancer patients who contract coronavirus.
Oncologist Dr Larry Hayward said: "Many of our treatments can suppress the immune system to some degree.
"So there was an initial assumption across the world I think, that our patients might be particularly vulnerable. But we've been keen to recognise this as an assumption only. We're also engaged in research UK-wide to try to understand in reality what it means."
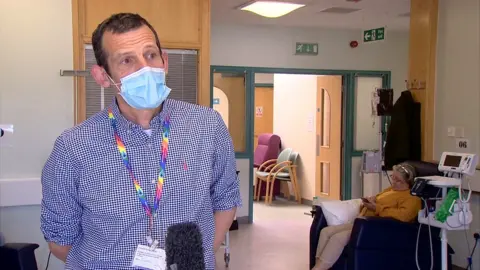
He added: "The picture is wider than merely the cancer. There's also the other illnesses that patient might be suffering from, the other past history of that individual, so we're having individual discussions of the risk and benefit of our treatments in the new Covid-19 world.
"Our estimate to date is that the Covid-19 issue isn't a dramatic extra risk as against the existing known risks of our treatments, and that's a really important message. It's one of the reasons we're able to get on with treatment in many patients."
Dr Hayward says the biggest impact has been on cancer surgical services.
Reduction in surgical activity
Of the approximately 32,000 patients diagnosed with cancer every year in Scotland, about 12,000 are usually sent for surgery as their first line treatment. But 85% of cancer specialists who were surveyed by the Royal College of Surgeons of Edinburgh in April said they were carrying out fewer cancer operations.
"There's been a significant expansion in intensive care provision," says Dr Hayward, "and that's had to use some of the highly trained theatre staff and some of the space in recovery and theatres to allow for that, so there has been a reduction in surgical activity."
He also echoed concerns from the interim chief medical officer Dr Gregor Smith, about a fall in the numbers of people being referred for urgent cancer tests, which could result in later diagnosis and poorer survival rates.
"A concern that we have is whether new patients are presenting as we'd hope they would with concerning symptoms to their GPs. The influx of new patients that we're really keen to see early in the course of their disease might be falling off if patients are too anxious to see their GPs in the context of the Covid-19 pandemic."

Meanwhile national programmes to detect breast, bowel and cervical cancer early have been suspended indefinitely.
Janice Preston, Macmillan's head of services in Scotland, says people need to know when operations and screening will restart.
"The anxiety that people have over cancer is real," she says. "People on treatment are frightened of getting coronavirus, or of their cancer getting worse if their treatment is altered or delayed. So we need to do as much as possible to address those fears and make sure people know what to expect."