Is Scotland's NHS ready for winter?
 Getty Images
Getty ImagesScotland's health secretary is preparing to announce measures to get the NHS through the winter.
Humza Yousaf has warned the coming months will be "extremely challenging" as the fallout from the Covid pandemic continues to affect services.
He will address MSPs on Tuesday, detailing measures the Scottish government will take to support the health care system over the coming months, as well as updating on progress of the NHS recovery plan announced last year.
However, bosses and frontline staff are already worried because pressures like longer A&E waiting times have come in the summer - ordinarily the quietest period of the year.
"Seasonal illnesses" like flu and norovirus mean more people will require care in the winter months and more NHS staff will be off sick.
Experts are warning about the risk of a big and early wave of flu and Covid has never gone away, with the UK Health Security Agency suggesting the autumn wave of the virus is already under way and putting pressure on the NHS.
So what are the biggest challenges?
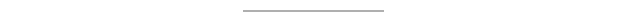
A&E waiting times can be a barometer for the pressures facing the wider NHS and many emergency departments are operating well below the Scottish government's target of having 95% of patients discharged or admitted within four hours.
The latest Scotland-wide average shows 66.2% of patients were dealt with within the four-hour target.
However, the length of A&E waiting times often depends on where you live.
Scotland's bigger hospitals, which attract the largest number of patients, are struggling the most. Edinburgh's Royal Infirmary was the worst performing in the week ending 18 September, with 45.8% of people seen within four hours
In the same week, 96.7% of patients attending Perth Royal Infirmary were seen within four hours.
This contrasts with Forth Valley Hospital near Falkirk which was at 46.3%.
Forth Valley, which was scoring around the 90% mark before the pandemic, was one of a number of emergency departments recently singled out by Mr Yousaf as having performed particularly poorly.
However, NHS Forth Valley is one of the best-performing boards in Scotland when it comes to outpatient appointments, so A&E waiting times do always not tell the full story.
Regardless of where they are on the scale of delays, nearly every emergency department in Scotland will have experienced issues in recent months with moving people out of A&E, staffing shortages, and patients with more complex needs.
None of these issues show any sign of abating in the winter months.
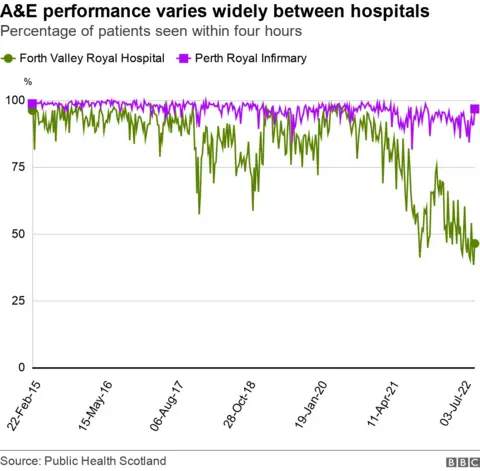
The number of deaths in Scotland has mainly been above average levels since the start of the Covid pandemic.
The count of what is known as "excess deaths" had been beginning to rise before 2020 and there are other factors at play too, such as an ageing population.
But in both 2020 and 2021 there were more excess deaths than usual with Covid, cancer and heart disease among the main causes.
There were fewer deaths than usual from respiratory diseases, such as asthma and chronic obstructive pulmonary disease, but National Records of Scotland says this is likely because many people who died with Covid had pre-existing respiratory diseases.
The recorded location of the excess deaths shows there are more deaths at home than we would normally expect.
This has seen higher percentage increases than hospitals or care homes, but the reason is not yet 100% clear.
Actuary Stuart McDonald, who has been monitoring excess deaths throughout the pandemic, told the BBC's More or Less programme that pressure on the NHS was "the strongest hypothesis for the current excess deaths we are experiencing".
If people are being diagnosed and treated later than usual then it means some are turning up at hospital with more complex and demanding medical needs.
In addition, Jillian Evans, head of health intelligence at NHS Grampian, has warned the cost of living crisis will strain Scotland's under-pressure healthcare services this winter.
She is worried people who cannot afford to eat well or heat their homes will be at greater risk of illness.
Another impact on the NHS this winter is trying to accommodate the sheer number of extra people waiting for treatment.
As of June this year, 451,020 new outpatients were waiting to be seen - 46.4% higher than the pre-pandemic average.
And around half of these people had been waiting more than 12 weeks.
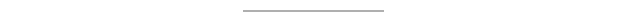
Some specialities face bigger challenges than others.
Across Scotland, 14.5% of inpatient paediatric surgery patients have been waiting more than two years for treatments, while 10% of urology patients have been waiting as long.
The number waiting for treatment for planned procedures such as knee or hip operations has increased by more than a third since the Covid pandemic began in March 2020.
One of the medical concerns about these delays is patients developing more serious health issues while they wait.
For example, the mobility issues of someone waiting for a hip operation can be more keenly felt in winter.
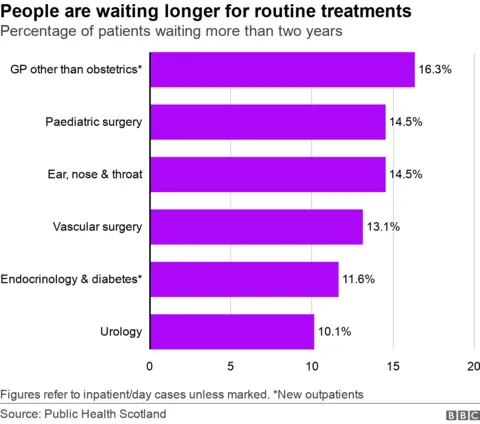
Bed-blocking or delayed discharge - where a patient continues to occupy a hospital bed despite being well enough to leave - continues to cast a shadow over Scotland's health service.
Latest figures show the average daily number of delayed beds in Scotland is 1,806 - with the NHS Greater Glasgow and Clyde area accounting for 368 of them.
Bed-blocking is a longstanding challenge for the NHS but one felt more acutely now because of a post-Covid lockdown increase in demand and a lack of available social care places in the community.
There are also fewer beds available.
Public Health Scotland data shows that in 2021/22, the average number of available staffed beds for acute specialties was 13,323 - a 2.4% decrease from 2016/17.
It also shows that, on average, 84% of the available staffed beds were occupied.
Caroline Lamb, chief Executive for NHS Scotland, told Holyrood's health committee: "We are heading into this winter with a situation where our hospitals are running at higher occupancy levels of their beds than we would ideally want."
If bed occupancy levels are already high then it leaves less wriggle room when it comes to finding space for the patients who come with the winter increase in demand.
A 'knackered' workforce
 Getty Images
Getty ImagesOne of the other issues is having enough medics to be able to safely care for the people in the beds.
As the health secretary has acknowledged, dealing with the pandemic has left many NHS and social care workers "completely knackered".
The knock-on effect from this has been difficulties in hiring and retaining staff in some areas.
The number of health workers is rising, and the current 155,182 NHS Scotland employees is 11.7% higher than five years ago.
But in critical areas, such as nursing and midwifery posts, the vacancy rates remain high.
In addition, the 11,838 people who left the NHS last year was a 10-year high and nearly every health board is experiencing above-average sickness rates. For example, the NHS 24 absence rate was 8.5% in March.
These pressures are always felt more keenly felt in winter and Scottish ministers have another potential challenge to contend with in the coming weeks with the prospect of strike action.
Healthcare staff from five unions are being balloted on industrial action after rejecting a 5% offer from the Scottish government. Ministers said they were "re-engaging" with unions over a deal.
