NHS Scotland deal signed for mesh removal surgery in US
 BBC
BBCThe Scottish government has signed a contract to allow NHS patients to visit a US expert for mesh removal surgery.
Patients can request the surgery with Dr Dionysios Veronikis in Missouri, with their travel and accommodation costs also paid for by the NHS.
The cost of each procedure is estimated to be £16,000 to £23,000.
Transvaginal implant use was stopped in Scotland after hundreds of women were left with painful, life-changing side effects.
NHS National Services Scotland said it would work with NHS Greater Glasgow and Clyde and local health boards to take forward arrangements for those who wish to travel to the US for the procedure.
The contract with Gynaecologic and Reconstructive Surgery of Missouri, where Dr Veronikis operates, follows a similar contract agreed with Spire Healthcare in Bristol earlier this year.
Mesh survivor Maureen Kane welcomed the move and told BBC Scotland she hoped to be allowed to travel to Missouri.
"I believe Dr Veronikis has the tools and techniques to be able to do it," she said.
"Once it's out, it can't do me any more damage. I'm hopeful my body won't be in any danger any more."
Maureen, from Lochgelly in Fife, was given her implant 11 years ago and suffered years of pain since.
A private scan in 2018 revealed wear and tear to the mesh. She was later told it had folded and broken.
She said she was desperate for surgery in the US, but had concerns over how soon it would be available for patients.
"It's ridiculous the time it has taken to get to this point," she said.
"I'm hopeful - but it's the timescale on how long it will take, how easy the process will be, and what the aftercare will be when we come back.
"This ruined a relationship for me, I was 50 when it was put in, I could be single the rest of my days now because of this."
 Mercy Hospital
Mercy HospitalHealth Secretary Humza Yousaf told BBC Scotland that he was determined for women like Maureen to "get the treatment they want and need".
Mr Yousaf said: "We have a menu of options for mesh survivors to choose from and all of them paid for by the NHS.
"You can get it here on the NHS in Scotland or you can go to independent contractors in England.
"Or if you preference is for Dr Veronikis, which I know is the case for many, then we now have that option to go to the United States."
Mr Yousaf said the overall cost of the scheme was expected to reach £2m to £3m. This includes reimbursements for women who have already paid for private surgery.
But he said there would be no cap on the funding that would limit the number of patients able to go to the US.

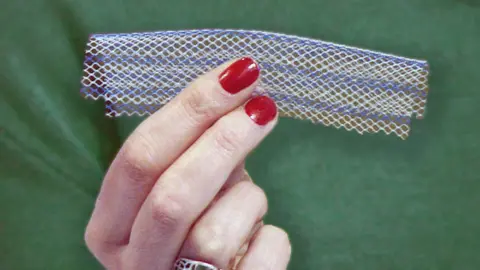
What are mesh implants?
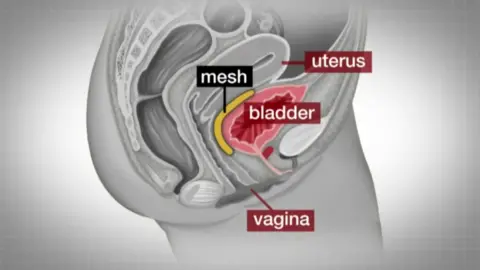
- The mesh, usually made from synthetic polypropylene, is intended to repair damaged or weakened tissue
- Over 20 years, more than 100,000 women across the UK had transvaginal mesh implants, which are used to treat pelvic organ prolapse (POP) and stress urinary incontinence (SUI), often after childbirth
- While the vast majority suffer no side effects, the use of mesh in Scotland was suspended except in "exceptional circumstances" in 2014 after it emerged some women suffered agonising side effects
- Use of the procedure was halted in 2018
- Once the mesh is implanted, it is very difficult to remove

Thousands of women have been given transvaginal mesh implants in Scotland to treat incontinence and prolapse - conditions many suffer after childbirth.
Some paid thousands of pounds to get private treatment to alleviate their symptoms.
The Transvaginal Mesh Removal (Cost Reimbursement) bill was passed by the Scottish Parliament In January to enable those who had already paid for private surgery to recover costs.
Mary Morgan, chief executive of NHS National Services Scotland, said: "This is a positive step in improving the range of patient pathways available to women injured by mesh.
"The options now available mean that mesh-injured women benefit from a service that has been designed to address their concerns and improve their experience."
Scottish Conservative MSP Jackson Carlaw said it was a "moment of huge relief" for those who had suffered so much.
He added: "This is another significant step forward for the brave women who have campaigned tirelessly to fight for justice."
