Mesh patients say they were 'duped'
 BBC
BBCTwo patients who were part of the review group looking at the safety of mesh implants were "duped" and "cynically used", MSPs have been told.
Mesh survivor Elaine Holmes said she and fellow patient Olive McIlroy were kept on the Scottish group to make its final report appear "less biased".
Ms Holmes appeared before Holyrood's Public Petitions Committee.
They called for MSPs to ensure the current suspension of mesh procedures "remains firmly in place".
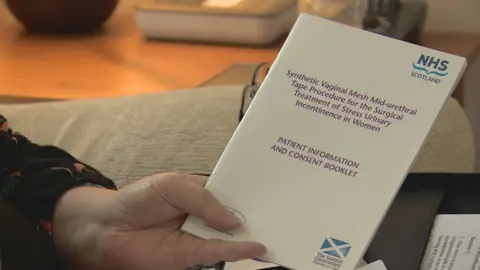
Transvaginal mesh implants are medical devices used by surgeons to treat pelvic organ prolapse and incontinence in women, conditions that can commonly occur after childbirth.
Severe complications
Over the past 20 years, more than 100,000 women across the UK have had transvaginal mesh implants - including more than 20,000 in Scotland.
But some have suffered painful and debilitating complications.
There are more than 400 women currently taking legal action against Scottish health boards and manufacturers as a result of mesh implant surgery.
In 2014, former Scottish Health Secretary Alex Neil called for the suspension of such procedures, and an independent review group was set up to look at safety issues.
Ms McIlroy, from Renfrew, and Ms Holmes, from East Renfrewshire, who both suffered severe complications following mesh implant surgery, were patient representatives on the independent review group.
They quit earlier this year claiming that the final report had been watered down.
Ms Holmes told the Holyrood committee the report was a "whitewash".
"We were cynically used to make the report appear less biased to the public and to those of you here today," she said. "We were duped, used.
"We are not politicians, doctors or statisticians, we are ordinary women horrified by failure rates of an operation and the severity of injuries that can be life-changing and life-threatening."
'Not in our name'
Ms Holmes said they went to Health Secretary Shona Robison before the report was published to ask her to delay publication until their concerns were investigated.
"It was to no avail. She accepted the final report and its conclusions, ignoring our concerns and publishing the final report just 11 days after our meeting. Any hope we had for change was completely dashed," she said.
Ms Holmes said the final report was "not in our name".
Public Petitions Committee convener Johann Lamont later said the evidence raised a range of "very concerning" issues about the process that produced the report.
She said a "lack of respect and credence" appeared to have been given to patients' views and experiences.
The Labour MSP said a debate had been secured in the Scottish Parliament chamber and she had written to the health secretary.
Catherine Calderwood, the Scottish government's chief medical officer, said "The patient representatives are the reason this review was carried out.
"They bravely came forward to tell their stories so it's extremely disappointing to hear that they do not feel they've been listened to.
"I've met with them several times and I certainly have heard their concerns and the harm they suffered with mesh."
During her evidence, Ms Holmes also attacked medical watchdogs MHRA (Medicines and Healthcare products Regulatory Agency).
She said it was "toothless and far too close" to manufacturers of medical devices.
"We need new health watchdogs who will insist on proof to show that devices and medicines are safe and effective," she added.
Less than satisfied
Committee member Alex Neil, who dealt with issue when he was health secretary, said this was the third scandal in the past few years where the MHRA's role had been "less than professional or helpful".
He said: "One of my concerns is that part of the funding does come from manufacturers of the device.
"I don't see how you can be independent regulator if you are, even partially, funded by the people who are being regulated. The independence of the MHRA is partly the problem."
The SNP MSP said he was less than satisfied when dealing with the regulator.
"I don't think they are a very professional organisation, I don't think they are a very caring organisation, I don't think they care at all about Scotland and I don't think they have got patient care as their number one priority," he said.
An MHRA spokesman said the watchdog protected the health of millions of people every day through the "effective regulation of medical devices and medicines, underpinned by science and research".
He denied that its role was "to protect industry interests" and said 90% of its funding came from the Department of Health.
He said patient safety was "our highest priority" and said the organisation sympathised with women who had suffered complications after surgery.
"We have undertaken work to assess the findings of studies undertaken by the clinical community over many years, as well as considering the feedback from all sources in that time," he said.
Cheaper than alternatives
He added that evidence supported the use of the devices in the UK for treatment of incontinence and organ prolapse in appropriate circumstances.
"In common with other medical device regulators worldwide, none of whom have removed these devices from the market, we are not aware of a robust body of evidence which would lead to the conclusion these devices are unsafe if used as intended," he said.
When the review was published in March, it concluded mesh implant procedures must not be offered routinely to women with pelvic organ prolapse, that patients should be offered a range of treatments - mesh and non-mesh - and they must be given the information to make "informed choices".
Dr Wael Agur, a clinician who also resigned from the review group, said the report had "left the door slightly open" for some procedures to be performed.
He told MSPs that mesh should only be used in exceptional circumstances due to the risks.
Dr Agur also told the committee that mesh tape procedures were cheaper than the alternatives, saving the NHS "significant amounts of money".
He called for the report to be opened up to a public consultation process.
The report is currently being independently reviewed by Alison Britton, a professor of healthcare and medical law.
