Covid inquiry: Former first minister says UK should have made NI decisions
 Belinda Jiao/PA
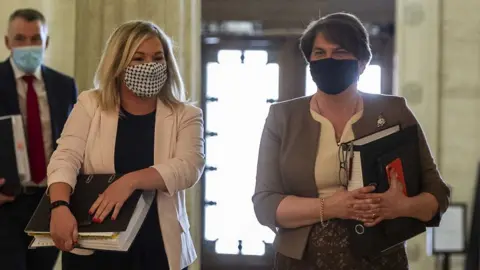
Belinda Jiao/PAFormer Stormont first minister Baroness Foster has said the UK government should have stepped in to make decisions in the absence of ministers at Stormont.
She was giving evidence to the UK Covid-19 inquiry on Tuesday.
Northern Ireland's devolved government did not function from January 2017 to January 2020.
Health officials have argued this affected Northern Ireland's preparedness for health emergencies.
The inquiry is focusing on Northern Ireland this week and its preparedness in the run-up to the pandemic.
Former deputy first minister Michelle O'Neill is scheduled to appear on Wednesday.
'Gap in resilience'
Baroness Foster told the inquiry Northern Ireland ministers "could and should" have been in charge of Stormont's government departments in the lead-up to the pandemic.
However, she pointed out that the Northern Ireland Office "took a policy decision not to intervene at that time" and instead left Northern Ireland "without any ministerial cover".
"Because of course we are a devolved administration - the Westminster government is sovereign at all times," she told the inquiry.
"And if there is a deficiency in the Northern Ireland administration then those people in Westminster with responsibility for Northern Ireland have a responsibility."
She added: "If there is a gap in resilience in part of the UK, surely that should concern the government of the UK."

Baroness Foster used this platform to stress the absence of Westminster politicians in the running of Northern Ireland.
On several occasions she told the Covid-19 inquiry that the lack of input made Northern Ireland less resilient when the time came to facing a major health emergency.
Referring to the time as "realpolitik", Baroness Foster said in the absence of power sharing the responsibility lay with Westminster to "step in".

Baroness Foster highlighted that in October 2016 a report from Professor Rafael Bengoa had recommended changes to the health service in Northern Ireland.
She said that all parties saw this as a "necessity" but following the collapse of Stormont in January 2017 this was not implemented.
Last week, Robin Swann, who served as health minister during the pandemic, told the inquiry a lack of reform and investment in the health service hindered its response to the pandemic
Baroness Foster said she was proud of the response of the Northern Ireland Civil Service and the health service to the Covid pandemic, especially in the absence of ministers.
However, she added that she was unsure if any amount of planning would have left Northern Ireland "fit for purpose" to deal with the Covid pandemic due to its scale and nature.
"The number one risk on the risk register across the UK was for a flu pandemic and what came towards us was not a flu pandemic but a very transmittable disease in the community," she said.
"Therefore the need to scale up and have the capability to deal with that was something we had to dig very deep into very quickly."
Work continued at Stormont
Giving his evidence, former permanent secretary at the Department of Health, Richard Pengelly, rebutted any suggestion that nothing happened in the absence of Stormont minsters.
He said that "preparatory work" continued but any strategic change required ministers in place.
"In that three-year period there were no issues about the work we were doing in the department as regards the development of our emergency response plan or emergency preparation that had a minister been in place, they would have landed on the ministers desk."
 PA Media
PA MediaThe first phase of the inquiry is looking at how prepared the UK and the devolved institutions were for the pandemic.
It plans to hold hearings until at least 2025, but updates and reports will be published by its chair Baroness Hallett as it continues.
On Monday, Northern Ireland's Chief Medical Officer Sir Michael McBride told the inquiry there was "no doubt" the absence of ministers had a significant impact on Stormont's preparedness for a pandemic.
He added Brexit also affected pandemic planning, with resources diverted to aid with implementing changes.
There was also a "very significant" shortfall in resources and staff to deal with the response required, the chief medical officer said.
