Belfast experimental cancer centre to get £1.7m research funding
 Tim Kerr
Tim KerrA man who was diagnosed with cancer in 2012 has said he "owes his life" to advances in treatments made by a cancer centre in Belfast.
The Experimental Cancer Medicine Centre (ECMC) is now set to receive almost £1.7m over the next five years.
The money is the result of a partnership between Cancer Research UK and the Public Health Agency in Northern Ireland.
The Belfast ECMC is part of a network across the UK, funded by the charity.
It delivers clinical trials of promising new treatments.
Since the network was first established in 2007, about 30,000 patients have taken part in 2,100 trials of new therapies.
They have included experimental immunotherapy, where treatments use the patient's own immune cells to try to fight cancer, and medicine trials.
The renewed funding for research was in part due to the role Tim Kerr, from Holywood, played in the grant application.
The father-of-three told his story to the panel as part of the scientists' pitch on what they would do with the money.
"Research, to me, is the way forward for work towards a cure," he said.
"Looking back at 2012 when I was diagnosed, I'm pretty sure if it had been 10, 15 years earlier, I wouldn't be here.
"The advances that have been made in treatments, early detection and surgery, in drugs and medicine in particular, which is what the ECMC is involved in, has got me to where I am, so I owe my life to those people who are dedicated to doing this sort of research."

The 65-year-old was diagnosed with stage four bowel cancer in 2012.
Stage four is when the cancer has metastasised to other organs, and in Tim's case it had spread to his liver.
"When I was flat on my back being treated here in Belfast, I know my surgeons were constantly in touch with people throughout Europe and in the United States, talking to them about my situation - how they would deal with it, comparing notes and so on," he said.
"Those sorts of advances didn't exist 15 or 20 years ago."
A year after his treatment, the cancer was detected again on his liver and in another surgical advance he had 70% of the organ removed.
He ended up spending more than a fortnight on life support, a month in intensive care and another couple of months on the ward learning to walk again.
That was followed by a lung tumour in 2016.
"I don't think it gets any easier any time someone says the words to you, 'You've got cancer'," he said.
"It just ripples through the family, the children. It's very hard to compute and process, and it's a devastating thing for anyone to have to contend with."
Seven batches of maggots
Tim also benefitted from other research advances, when a clot on his leg resulted in a troublesome and long-lasting wound.
"One of the treatments they gave me was the application of maggots," he said.
"I had seven batches of them. They come in a little perforated teabag. They go in the size of a pinhead and come out the size of a small worm, having done a remarkable job of taking care of all the dead skin and debris that exists around a difficult wound.
"They did attract a good audience on the ward!"
Now, his wound long healed and five years on from his last surgery, Tim's risk of developing cancer is the same as anyone who has never had the disease and he is making the most of life.
"I've enjoyed taking up baking bread, fermenting foods, taking more exercise - living.
"It's good to be alive."
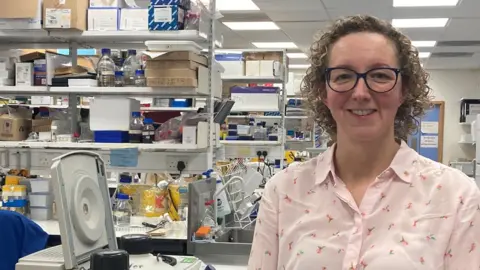
Dr Vicky Coyle, a clinical professor and medical oncologist at the centre, said the funding would be critical in advancing cancer management and making new and existing treatments more effective.
"It's really important for our patients because it gives them access to clinical trials," she said.
"And it's also important for us because it brings our research, started in our labs here in Belfast, through to clinical trials to benefit patients in Northern Ireland and beyond."
Any treatment plan offered to a cancer patient has been driven by research.
"Yesterday's experimental treatments or new treatments become today's standard of care treatments," said Dr Coyle.
"Some of those patients will benefit directly from taking part in the research, but as our patients often say to us, 'Even if it doesn't help me, it might help someone else'.
"And so they indirectly will be contributing to making outcomes better for many, many other patients for years to come."
Dr Kienan Savage, the scientific lead at the centre in Belfast, says Tim's story is "testament" as to how far cancer treatment has come over the years.
"Tim has been instrumental in actually getting this funding across the line," Dr Savage told BBC's Good Morning Ulster programme.
"Particularly in terms of helping us articulate to patients how important this research is but also helping us design trials and make sure we're getting the most out of those trials for patients.
"Today's trials and research will become tomorrow's treatments so we need to make sure we actually do the best research for patients and Tim really helps us to find that and refine that."
