Borderline personality disorder: 'I found my lost tribe and faced my fear'
Marie Coyle had her first panic attack when she was seven years old.
Her mental health deteriorated further after a traumatic experience when she was 21, and she has since battled anorexia, anxiety and post-natal depression.
But it wasn't until she was in her 40s that Marie received a mental health diagnosis, which "finally made sense".
Marie, from County Down, was diagnosed with borderline personality disorder (BPD).
Marie said she was shocked when she was presented with a list of BPD symptoms by a psychiatrist and realised she could "tick every box".
According to the NHS, symptoms vary and may include emotional instability, disturbed patterns of thinking or perception, impulsive behaviour and unstable relationships.
"For the first time in my life I realised there was something I could put a name on. I was given the answer," Marie said.
"It was like I was living on high alert at all times."
Marie was advised by her mental health team that she could benefit from specialist talking therapy known as dialectical behavioural therapy (DBT), which is specifically designed to treat people with BPD.
It is particularly effective in treating women with BPD who have a history of self-harming and suicidal behaviour.
'Light at the end of the tunnel'
Although Marie faced "a lonely and very hard" two-year wait for the treatment, she said it eventually led her to experience "pure joy" for possibly the first time in her life.
"Through the therapy I had to face my fear, to keep going and work through the negative stuff and question it," she said.
"I realised there was light at the end of the tunnel."
Marie said she wished DBT was more widely available. Her call has been echoed by Northern Ireland's mental health champion Prof Siobhan O'Neill.

What is borderline personality disorder?
Borderline personality disorder (BPD) is a disorder of mood and how a person interacts with others. It's the most commonly recognised personality disorder.
Research shows that about one in 100 people live with BPD.
BPD is sometimes called emotionally unstable personality disorder (EUPD). Some people feel that this describes the illness better.
In general, someone with a personality disorder will differ significantly from an average person in terms of how he or she thinks, perceives, feels or relates to others.
There are different reasons people get BPD.
A lot of people who live with a diagnosis of BPD have had traumatic experiences in their childhood.
SOURCE: Rethink Mental Illness

Prof O'Neill said DBT often worked for the disorder when other treatments had failed.
"BPD is one of the more stigmatising mental health illnesses and is very difficult to diagnose," she said.
"DBT has been rolled out in Northern Ireland but it can be difficult to get the treatments people will benefit from. Getting the right therapy is a prize worth holding out for."
Prof O'Neill and Marie have both expressed discomfort around the title BPD, which is contested.
Prof O'Neill said the label suggested there was something fundamentally wrong with the person rather than a "series of behaviours a person has developed to help them deal with trauma".
Six years after her own positive experience of therapy, Marie continues to attend a peer group for those with the same condition, which she said has been like finding her "lost tribe".
'We're all human'
"The first time I went to the group was nerve-wracking but I made it to the room and suddenly people were talking like me, saying what they were thinking and feeling.
"It was such a bonding experience.
"There can be people out there that are actually ashamed to say it [BPD] because of the stigma, when there's absolutely nothing to be ashamed about it. Everybody has emotions. We're all human."


DBT services across Northern Ireland
The availability of DBT varies across Northern Ireland's health trusts.
In a statement, the South Eastern Trust, where Marie accessed her therapy, said it hoped the therapy could be more widely accessed.
It said the Northern Ireland Personality Disorder Network was working on a business case for the Department of Health to ensure parity of access.
"If further resources were to become available, the trust could provide treatment to more people, more quickly, " the statement said.
Belfast Trust:
DBT is not available - the trust said it has "a small number of staff trained in DBT skills and they may use these within their practice".
Southern Health Trust:
DBT is available - it is offered as main treatment method for individuals diagnosed with BPD.
South Eastern Health Trust:
DBT is available - the trust said it "aims to commence treatment with DBT within six months of referral".
Western Health Trust:
DBT is available.
Northern Trust:
DBT is available - the trust said it has offered DBT as a treatment option for six years.

'It is life-affirming'

There is growing evidence that art can help in the healing process for those who have experienced trauma, according to Prof O'Neill.
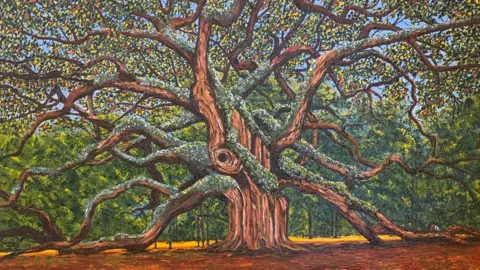
Marie has rediscovered her love for art, which she had given up as a younger woman, through a charity that offered art therapy. She said it had re-instilled her confidence.
She is now hosting her third public art exhibition since the first Covid-19 lockdown.
"The day I booked my first exhibition was the scariest moment of my life. I was putting my whole heart and soul out there and I knew that judgements would come."
 Marie Coyle
Marie CoyleBut Marie found the experience "life-affirming".
"I realised my fears were stopping me doing what I really wanted to do. Fear stops so many people doing what they want.
"I'm putting my story out there, trying to help somebody else.
"Everybody has some traumas, everybody has things that they're dealing with.
"Go get help, talk to your GP, talk to family, friends, talk to somebody. Get out there and get help for yourself because there is help."
Information and support about issues raised in this story are available on the BBC Action Line.
