Coronavirus: NI health service rebuild 'constrained' by pandemic
 PAcemaker
PAcemakerRebuilding Northern Ireland's health and social care system will be "significantly constrained" by Covid-19, the health minister has said.
Robin Swann has published a strategic framework for rebuilding health and social care services in the wake of the first wave of the coronavirus pandemic.
He said the service was in "very serious difficulties" before Covid-19.
"The virus has taken the situation to a whole new level," he said, and warned of a hike in cases as lockdown eases.
"Accessing retail, accessing leisure facilities, accessing tourism and hotels and all the rest of it over the next few weeks and months, there will be an increase in Covid cases in Northern Ireland," he added.
'We can't rush this'
His announcement came as no new Covid-19 related deaths were recorded in Northern Ireland for the third day in a row, with the Department of Health's death toll remaining at 537.
Its daily figures mostly comprised hospital deaths and where a patient had previously tested positive for the virus - and are lower those provided by government statistics agency Nisra which records all fatalities where Covid-19 was mentioned on a death certificate.
The health department recorded three new confirmed positive cases of the virus on Tuesday, bringing that total to 4,805.
Mr Swann described the figures as encouraging, but warned: "The situation is still finely balanced and we only get one chance at this phase, we must proceed gradually.
"I want people to get their freedoms back but we can't rush this."
Scaling up services
The five health trusts are to publish plans for tackling waiting lists, providing high-priority cancer services and dealing with other urgent conditions.
They have also plans for scaling up services in the immediate period until 30 June.
Telephone triage, video consultations and other measures used since the coronavirus outbreak will now be embedded in primary and secondary care, according to the minister.
"I don't want to simply restore the health and social system to the way it was at the beginning of 2020," said Mr Swann. "I honestly believe we can make it better."
He said this would require patience, careful planning, sustained investment and collective support, not just around the executive table but "across society as a whole".

Wanted: Vision, funding and political will
Analysis by Marie-Louise Connolly, BBC News NI health correspondent
The coronavirus pandemic has diminished the health service's already-drained budget while increasing hospital and cancer treatment waiting times.
There have been positives. The outbreak has prompted the introduction of more telephone triage and video consultations, for example, as well as Robin Swann's big vision proposal to rebuild Northern Ireland's health and social care system.
There is now a focus on social care, nursing homes and an increased will to get things done.
But the backdrop hasn't changed. The system remains bereft of staffing and, in some areas, leadership.
In order to deal with coronavirus, services were considerably scaled back, some moved to different hospitals, which led to a number of temporary closures including the Downe and Daisy Hill emergency departments.
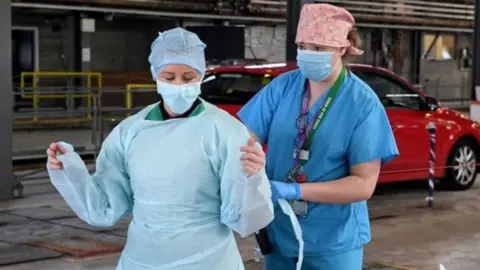
 PA Media
PA MediaWhile undoubtedly the measures - which included creating a Nightingale facility in Belfast - saved lives during the pandemic, many are asking at what cost.
As rebuilding services starts, plans will be hampered by the additional demand for personal protective equipment (PPE) across the system.
The department's budgetary position continues to be challenging.
All of this on top of preparing for the eventuality of a second wave of coronavirus.
Resuscitating services will require vision, planning, sustained funding and political will.

A new management board for rebuilding health and social care services has also been created, likely to consist of senior Department of Health officials, the chief executives of the health trusts and others.
Meanwhile, the Royal College of Emergency Medicine has said Covid-19 must trigger a "resetting" of emergency department care.
The Royal Victoria Hospital's (RVH) Dr Paul Kerr said the pandemic had created an opportunity to do things differently.
"There's a real risk of patients infecting each other and of infecting staff," he said.
The emergency department's waiting area at the RVH can usually seat 75 people but under the 2m rule, that number reduces to 22.
'A real challenge'
"It's a real challenge because people come in quite anxious and perhaps in a panic and we have to direct them to sit apart and in a certain direction," said Dr Kerr.
 PA Media
PA Media"Then there are relatives who might want to go in quickly to see a relative who is sick and that is too difficult because we have to restrict all of that."
The Royal College of Emergency Medicine has made a number of recommendations about how care in emergency departments should be delivered, including:
- Emergency departments should "not become crowded ever again" or "reservoirs of hospital acquired infections";
- Improving infection control;
- Reducing crowding and improving safety;
- Redesigning emergency departments and using Covid-19 testing for best care.
Mr Swann said he would review the use of specialist Covid-19 centres in Northern Ireland, and that they will now move to an on-call basis.
But he insisted the centres would be required in the event of a second surge.
"I am in no doubt - as we allow people to come back out into the normal way of life - that there will be an increase of Covid cases in Northern Ireland, and we need still the facility and the structure to support those people when they need it."
Eleven centres were set up during the height of the coronavirus pandemic as part of the Department of Health's "surge planning" to assess patients with suspected symptoms.