Dr Michael Watt: Neurologist 'carried out hundreds of needless procedures'
The suspended Belfast neurologist Michael Watt carried out hundreds of unnecessary procedures on patients, a BBC Spotlight investigation has revealed.
Dr Michael Watt worked at the Royal Victoria Hospital as a neurologist diagnosing conditions like epilepsy and Parkinson's Disease.
He is currently suspended from practising medicine.
Dr Watt was responsible for a huge spike in the number of epidural blood patches carried out in the Belfast Trust in 2015 and 2016.
A blood patch is a rare neurological treatment, usually for patients with a condition called spontaneous intracranial hypotension.
A report by the Department of Health, details of which have been obtained by Spotlight, says that almost none of the patients on whom Dr Watt carried out blood patches had the condition he was treating them for.
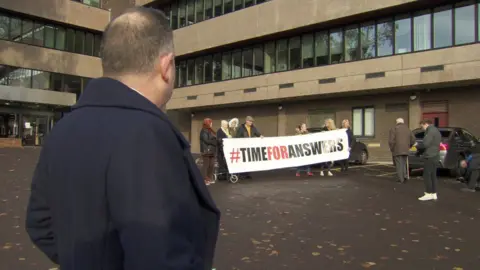
In 2018, almost 3,000 of Dr Watt's patients were recalled for a fresh assessment of their care.
Last week, Spotlight reported that one in five was told at the recall they had been misdiagnosed.
A blood patch involves injecting the patient's own blood into their spine.
Spotlight's research indicates that Michael Watt carried out 261 blood patches in a nine-year period from 2009 to 2017 inclusive, more than 160 of which were over two years, 2015 and 2016.
To put the figure in context, the programme sent a Freedom of Information request to 150 health trusts across the UK asking them how many blood patches they carried out in 2015 and 2016.
Ninety-six responded and analysis of their responses reveals that Michael Watt was carrying out more blood patches than any of them.
'Extraordinarily high'
A blood patch expert at the Countess of Chester Hospital in Cheshire, Dr Simon Bricker, told Spotlight that blood patches are normally done by anaesthetists.
He said the numbers being done by Dr Watt were "extraordinarily high" and "somebody doing epidural blood patches in very large numbers should raise red flags straightaway".
The programme also heard testimony which suggested Michael Watt may not have carried out blood patches in sterile conditions, which Dr Bricker said was "crucial" when doing a blood patch.
One patient, Therese Ward, described how she contracted meningitis after one of her blood patches, while another two were excruciatingly painful.
 Getty Images/fotostorm
Getty Images/fotostormDr Bricker told Spotlight that meningitis is a risk of a botched blood patch.
He added that the procedure, when done properly, should be largely painless.
'Traumatic experiences'
Therese Ward gave permission for the Belfast Trust to respond publicly to Spotlight's questions about her care.
Despite that, the Trust said it was unable to publicly discuss what it called the "personal and traumatic experiences" described by some of Dr Watt's patients.
It did not respond to questions about what it knew of Michael Watt's blood patches during the time of the spike.
It said that blood patches are carried out with an aseptic non-touch technique in a clean environment.
It added that a report into Michael Watt's care had recommended a new local guideline for blood patches which had recently been implemented.

Spotlight has also revealed that Michael Watt's enthusiasm for blood patches was first curtailed because of the intervention of a GP.
In late 2016, a Comber-based physician noticed that several of his patients were receiving blood patches.
He didn't think they needed them and told the Belfast Trust.
Six months later, in summer 2017, Dr Watt was removed from clinical duties.
The recall of patients followed an investigation by the Royal College of Physicians.
The Department of Health said that it is frustrated with the situation.
"While we fully recognise that the delay in the release of the outcomes report - for reasons outside our control - is hugely frustrating for former patients of Dr Watt, we must emphasise that all recalled patients will have had direct dialogue with clinicians as regards their own diagnosis," it said.
In early 2019, Dr Watt was suspended from practising medicine.
A spokesperson for the PSNI said: "We are aware of the recall of neurology patients by the Belfast Health and Social Care Trust and have met with senior officials within the Department of Health to discuss the issue.
"The Department has agreed to provide us with further information so that we can assess how best to move forward and to enable us to determine if any potential criminal offences can be identified."
