Weight loss unit 'could reduce stigma'
A weight loss surgery patient has said she hopes a dedicated weight loss surgery clinic in Northern Ireland will "de-stigmatise" being overweight.
Colette Donaghy, 39, says people can be "absolutely cruel" about obesity.
Last year's Health Survey, from the Department of Health, found that 64% of adults here are overweight or obese.
In March 2019, the department said it would assess if a weight loss unit should be created in Enniskillen.
Two-thirds overweight
Bariatric surgery, also known as weight loss surgery, is used as a last resort to treat people who are dangerously obese (having a body mass index of 40 or above or 35 plus other obesity-related health conditions).
The two most common types of weight loss surgery are:
- Sleeve gastrectomy or gastric bypass: Where some of the stomach is removed or the digestive system is re-routed past most of the stomach.
- Gastric band: Where a band is used to reduce the size of the stomach so a smaller amount of food is required to make someone feel full.
Ms Donaghy struggled with her weight for many years before deciding to have gastric band surgery privately in England in 2008.

She said that it was initially very successful and she lost 11 stone.
However, she struggled to maintain both the weight loss and, crucially, keep up the medical appointments which are needed afterwards.
"When the band goes in, there's still work to be done to get you to what they call the 'sweet spot' where there's just enough fluid in the band to restrict your eating, but you then do have to continue to maintain that," she said.
"After the first year, you have to pay for each individual doctor's appointment on top of having to take days off work and flights to and from Liverpool."
Vital after-care
Eventually, Ms Donaghy was not able to make the trips as often as she should, and the weight began to creep back on.
She said that if the surgery becomes available via the health service in Northern Ireland, the locally provided after-care and support will be vital.
 Getty Images
Getty ImagesThe County Armagh woman also said she believed the value offered to the health service balance sheet is clear.
"The amount of money it would cost to do these operations as opposed to the amount I could potentially cost the NHS if I became diabetic or had heart problems or blood pressure issues, it speaks for itself."
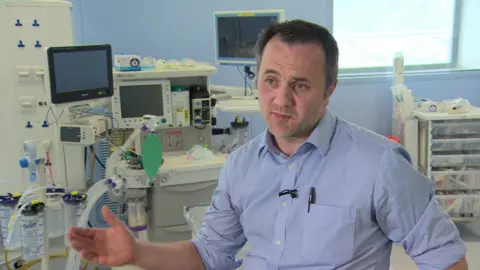
Dr Michael Mullan has performed bariatric surgery outside of Northern Ireland and is now based at the South West Acute Hospital in County Fermanagh.

He said it is a safe procedure which can be used in conjunction with changes to lifestyle and diet that can really enable people to "get their lives back".
"Your typical person will be 45-50, someone who was fit and active when they were in their twenties, then life got busy on them and then they struggle to get the weight off.
"You can find people who maybe for 20 years haven't been able to shop in a regular shop, became isolated at home, afraid to go out and about because they are embarrassed about their situation - so people get their life back with this operation."
Dr Mullan said obesity is an increasing problem here but stressed that surgery will not be the answer for everyone.
"This surgery is for people who have obesity-related medical conditions, who realise they need a change and need some help with that change. "
Running by 20
Consultant surgeon Mark Taylor, who is part of the Department of Health's group assessing the need for such a service, has said he is "confident" the service would be "up and running" by the start of 2020.
Obesity costs the local health service approximately £457m per year.
According to Dr Mullan, it will save the health service money in the long-run and for some people it will put their diabetes into remission.
On the issue of travel to Enniskillen, Dr Mullan said the "bottom line is people will be expected to travel".
"That's the way it's going to be after all at the moment they get on a plane and travel to England, Holland and France. Here we are asking them to travel to Enniskillen and it's on the National Health Service."

Ms Donaghy, who is once again dieting and exercising to lose weight, hopes that together with a bespoke surgical unit, there will come a more supportive attitude.
"None of us are in this position because we want to be," she said.
"Really it is a situation we have unfortunately got ourselves into, and with the best will in the world, we just can't get ourselves out of."
