Covid-19: Ipswich and Colchester hospitals' unsung heroes of the pandemic
 BBC
BBCDoctors and nurses in intensive care departments have shared their experiences throughout the pandemic, but what of the army of staff who have worked behind the scenes to keep hospitals running? The BBC spoke to three people about the highs and lows of the past year.

'I was perceived as a threat'
The Reverend Linda Peall has had, as she puts it, a "rollercoaster" year.
She began her new role as head of the chaplaincy service for Ipswich Hospital and Colchester Hospital in February 2020, just before the UK's first coronavirus lockdown in March.
When people needed her support more than ever, it was no longer safe to walk from ward to ward to chat freely with patients, visitors and staff.
"We're here for everybody - people of faith, people who don't have a religious belief - to support people on their journey, listening to them, being with them," she says.
"We've had to completely change how we work."

She and her team have relied on referrals for patients from relatives, faith leaders and staff, but with the latter often being too "overwhelmed" to do so.
In supporting staff, Ms Peall says: "We've had to help them reconnect with those values [that brought them into health care], realise they are doing the best in difficult circumstances, and that's enough."
With visiting off-limits, much of her role has been to reassure families and loved ones.
But even that came at a price.
A "very distressed" patient wished to speak to her husband, so the priest made the phone call and began by explaining who she was.
"His immediate response was 'Who are you? Why are you in my wife's room when I can't be there with her? Have you got Covid and are you going to give it to her?'," says Ms Peall.
"I will never forget that, as long as l live.
"I've never experienced a time as a chaplain where I was perceived as a threat and somebody who might do harm to someone."
From that "difficult encounter", she reflects more positively on the teamwork that culminated in her holding an iPad so a patient could watch a live stream of his wife's funeral.
"He commented to me about his wife, how much he loved her and how amazing she was," she says.
"That privilege of being with somebody in that most personal and important moment - that, for me, has been the highlight of the pandemic."

'There was a lot of anxiety, a lot of frustration, a lot of sleepless nights'

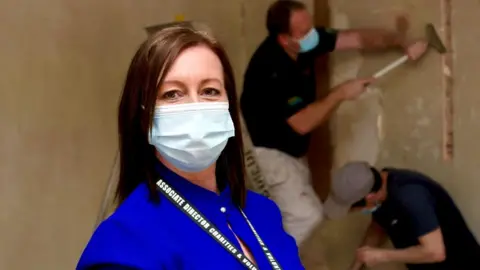
The logistics of a hospital's response to a pandemic falls on the shoulders of people like Shume Begum.
She is part of a team that relocates equipment, beds and staff to where they are needed.
"It's been really challenging," says Ms Begum, who was only three months into her role as an associate director of operations when the pandemic hit.
"We had to adapt to new ways of working - communication was key, and things were changing really rapidly," she says.
Among the changes were expanding critical care units to ensure they could go well beyond their normal capacity.
"We had to ensure we had the infrastructure, the equipment, that the environment was set up, bring the clinical operations together," she says.
"Luckily in the first surge that didn't happen, but during the second surge, we went over 200% of normal capacity.
"We had to bring staff in who hadn't worked in critical care, so there was the training element of that and ensuring other areas where we'd redeployed staff were safe."
'Covid is here to stay'
She described a "culture change" among the workforce of adapting to new rotas so the hospital could take more patients.
"There was a lot of anxiety of how we were going to do this, lots of sleepless nights," she says.
"We had tears of frustration of wanting to get everything moving really quickly.
"[But] having the teams around you has made me get through - and feel privileged to be part of it."
She says the hospital and staff are entering a period of reflection.
"Covid is here to stay," she says.
"We are all going to be looking at what the new normal is and how we cope.
"Seeing teams so easily conforming to what they had to do, knowing they were dealing with the sickest patients, and being part of a team ensuring they had the equipment to do that, was a high point for me.
"The care those patients got was outstanding. I feel our teams have gone way over and above."

'I don't think we've seen anything like it before in terms of volume of gifts for staff'
Mandy Jordan was well used to co-ordinating fundraising for Ipswich and Colchester hospitals before last year, less so in dealing with a delivery of 5,000 Easter eggs.
"Someone thought 'what do nurses really need? I know, chocolate'," laughs Ms Jordan when recalling a surprise delivery.
As director of charity and voluntary services, she had been promoting the need for a new breast cancer centre and revived children's department.
Then the pandemic hit and she was helping distribute treats, personal protective equipment (PPE) and donated hot meals among 10,000 staff.
"At first it was food that started to pour in and there were lots of reports of a lack of PPE and people decided they would make everything," she says.
"It was dealing with the logistics, and you're talking thousands of masks and thousands of visors coming in on a daily basis."
The charity team sifted through what was useful and compliant.
"It was overwhelming," she says.
"We didn't know what was coming in and we didn't know what we needed either. There was so little information.
"We had gone from organising fun events... to logistics for something enormous."
As food businesses closed during lockdown, many offered surplus stock or meals, with donations distributed as fairly possible.
"I don't think we've seen anything like it before in terms of volume of gifts for staff," says Ms Jordan.
Generosity is key. Whether its thousands of Easter eggs, a hot meal or people's time or money, the pandemic has seen it all.
Applications for voluntary work at the hospitals topped 500 and a wellbeing fund, boosted by NHS Charities Together, will mean almost £700,000 is put towards mental health and financial support for staff and towards creating two non-clinical break areas away from the wards.
"What we can learn is that our communities do pull together in a time of crisis," says Ms Jordan.
Photography by Martin Giles

Find BBC News: East of England on Facebook, Instagram and Twitter. If you have a story suggestion email [email protected]