Somerset health bosses spend £6m to free up hospital beds
 BBC
BBCA county's health bosses are spending more than £6m to get patients out of hospital and back into the community.
NHS Somerset hopes investing in a range of schemes, including care for up to 300 patients in their own homes, will help free up hospital beds.
It comes as hospital's face intense pressure and increased wait times.
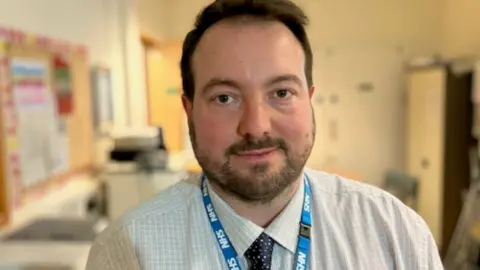
Chief executive of the Integrated Care Board, Jonathan Higman, said supporting people in the community will also help them "live healthy lives for longer".
Amongst the schemes being rolled out are "virtual wards", that provide care in people's own homes, and a mobile GP service.
Figures for October show 57% of patients had to wait more than four hours in the emergency department at Musgrove Park Hospital in Taunton before being discharged, but there had been a 10% improvement in November after many of these schemes started.

Guy Mock, 41, was admitted to Musgrove Park Hospital after suffering abdominal pains.
After being seen quickly initially he then faced more than 10 hours on a trolley waiting for a bed to become free.
This was despite the fact that 95 out of the hospital's 569 beds contained patients who were fit to be discharged - there was just no place for them to safely go.
Outside the hospital, six ambulances were also waiting with patients who needed to be admitted.
Mr Mock said: "Everyone has been really kind and they triaged me really quickly. They have allowed me to lay down as sitting is more painful."
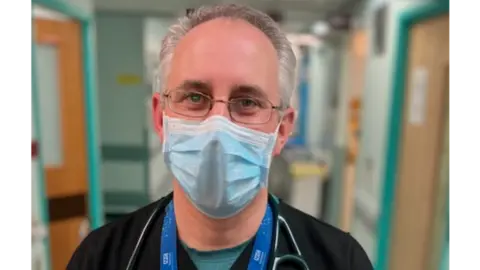
Dr James Gagg, the consultant in charge of emergency treatment, said it was not unusual to have 70 patients in the department.
"It would be unusual if you went back a few years but it's becoming increasingly normal for this winter," he said.
The £6m spend, which has come from the Government's 'Better Care Fund', means a range of new initiatives are now up and running to help the pressure on beds caused by Somerset's ageing population.
'Carry on as normal'
David Cox, 82, from Burnham-on-Sea, is receiving care through the Hospital at Home initiative.
Mr Cox said having treatment at home had allowed him "to carry on my life as normal".
The clinical lead for the scheme, Dr Charley Davies, said: "It is a service for adults who would otherwise be in hospital and it allows them, initially - those that have illnesses such as respiratory or frailty - to be treated at home rather than hospital."

Keeping patients out of ambulances is another way of reducing demand on hospitals.
South West Ambulance Service NHS Foundation Trust (SWASFT) was the first in the country to launch a mobile GP service.
Medical lead for the Somerset Ambulance Doctor Scheme, Dr Matthew Booker, said the service aims to complement the expertise and skills that frontline crews have, but also provide an additional level of care.
The doctors carry blood-testing equipment with them as well as an ultrasound unit.

"This is a portable laboratory where we can run patient's blood samples and often the types of tests that are done in the emergency department we can do on the vehicle," he said.
Dr Brooker added that this allowed them to "perhaps go further with a diagnosis than some of our paramedic colleagues can".
Health and social care funding is also being invested in care homes, like Gotton Manor near Taunton.
In just a few weeks, an old barn at the care home has been converted into a re-ablement centre providing nursing staff and therapy to get patients out of hospital and back into their homes within six weeks.
Though it is early days, it is hoped these schemes could already be having an effect on the demand for hospital beds.

Follow BBC West on Facebook, Twitter and Instagram. Send your story ideas to: [email protected]
