Intensive care delirium: 'I hallucinated that I'd been kidnapped'
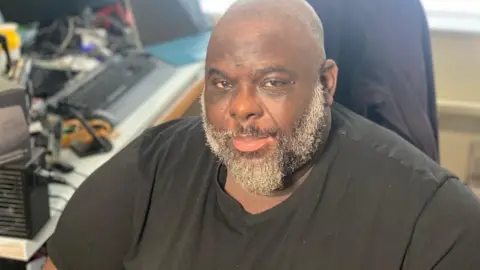
 Jan Ehtash
Jan EhtashWhen Jan Ehtash woke up she immediately began to panic. She was lying on her back, paralysed from the neck down and was terrified about what was happening to her.
"I thought 'I've been kidnapped, I'm here now, can't move, I can't talk and there's all these weird people walking around with great big helmet-type things'," she says.
Believing her captors were about to begin experimenting on her, the 58-year-old tried to work out how to escape. But all she could do was lie motionless, surrounded by strange machinery which continually beeped and whirred.
It was at that point she realised the machines had their own language.
"I thought they were communicating, these machines, they were communicating with each other," she says.
"It was just very frightening, it was so frightening."
But Jan hadn't been kidnapped and the machines were not talking. She was actually in an intensive care ward in a south London hospital having spent five weeks in a coma battling a Covid infection that had almost killed her.
It was January 2021. Her abductors were actually the doctors and nurses who had saved her life.
Her paralysis was only temporary and her hallucinations had been brought about by a surprisingly common phenomenon called intensive care delirium, or ITU delirium.
"Being admitted to intensive care feels - to the patient - similar to being imprisoned," explains Dr Larry Mulleague, an ITU consultant who treated Jan at St Helier Hospital, in Carshalton.
"There is an acute loss of control, as well as fear, great difficulty in being understood, and physical and emotional distress."
According to Dr Mulleague, ITU delirium affects more than half of patients at the trust, but the experiences of patients are rarely the same.
"Some of the luckier ones may imagine themselves as an extra character in a favourite book like Alice in Wonderland, but more frequently the hallucinations are very frightening with themes of being kidnapped, tortured, drowned, and spied on," he says.

Jan's journey to this strange world began several weeks earlier when she contracted Covid.
Struggling to breathe, she was admitted to St Helier Hospital having only brought a handbag with her, convinced that she would be discharged within a day.
Then a doctor told Jan, "We can't promise that you'll come out of this," and said she should call her family. It was Boxing Day.
"So I phoned up my husband and the children, which was horrific," she says. "My youngest daughter screamed down the phone and said, 'Mum, I can't lose you. You've got to fight this.'"
Nearly two years later, Jan still wells up thinking about that moment. "How can I say their mum isn't going to be around? I couldn't even give them a hug. It was a phone call."
 Jan Ehtash
Jan EhtashJan was sedated and put on a ventilator.
"She was probably one of the most unwell patients we had," explains Jessica Gregory, senior sister at St Helier Hospital's ICU. "We were extremely worried about whether or not she was going to survive."
It would be five weeks until Jan woke up to her strange visions.
She was eventually discharged from hospital with a carrier bag of medication and unsettling flashbacks from her time in a coma.
She recalled one of her daughters talking to her and another lying on her chest. She remembered being wrapped in a sheet and turned on her front whilst being ventilated.
All of these had taken place, but it was difficult to distinguish what was real from what was not.
She also found it difficult adjusting back to life at home. For a time she could only sleep if she played videos of the same beeping machines from intensive care on YouTube.
"It was a comfort in the end... I needed to hear those machines for some reason," Jan says.
Rhyan Fuller had a similar experience to Jan. He was induced for the same reason - a life-threatening Covid infection.
He had also not realised how close to death he was. But the 40-year-old business analyst's hallucinations were more prosaic.
"It was random things like speaking to people while I was outside next to the river. And I'm like, 'well there's no river in St Helier'," he says.
Rhyan also believed he'd recently collected his laptop from the second floor of the hospital.
"That's a really weird place to be in whilst you're trying to recover," he says.
While aspects like illness, age, medicines, noise levels and insomnia are thought to contribute to the delirium, research continues into its cause and how it can be treated and prevented.
"There are practical remedies that we provide in our hospitals - a window and a clock with a 24-hour face so patients can orientate themselves to day and night, quieter machine alarms," Dr Larry Mulleague says.
"We also offer early physiotherapy, frequently tell patients where they are, provide glasses and hearing aids, and play their favourite music. Hearing a familiar voice or feeling the touch of family members helps, too."
He adds about the importance of providing support to patients even after they leave hospital, with support groups and specialist psychologists on hand.
"Fortunately by the time we see them in our follow-up clinic three months after discharge, the rawness of those memories and the emotions they elicit have gone.
"But explaining how common these thoughts are for survivors is often the validation they, and their families, need," he says.

To help with their recovery, both Jan and Rhyan are part of a peer support group for those who have experienced ITU delirium, based at St Helier Hospital.
In a small room under fluorescent lights the patients discuss their close brushes with death and their hallucinations.
One woman explains how she thought she was magnetised to her bed, another says she kept seeing the American detective Columbo.
The majority of attendees have recovered physically and these sessions aim to aid their psychological recovery from intensive care.
"I went to the first group and they answered every question I had," says Jan.
"You're thinking, 'Am I normal? Am I going crazy?' But then you hear other people have experienced the same thing and you're like, 'Oh my god, it's not just me.'"

Maria Carroll, a senior ICU nurse, believes patients find it "very beneficial". The medics might understand their journey to a degree, she says, "but we haven't walked in their shoes. We don't get it like they get it, and they have something in common that they'll have in common with nobody else".
Rhyan agrees about the benefits of learning from other people's experiences.
"There are going to be people there who might say things that will make this entire journey a little easier to digest," he says.
"And there are also those that might want to hear, depending on how far along they are, that it's hard - it's really hard - but it does get better."

Follow BBC London on Facebook, Twitter and Instagram. Send your story ideas to [email protected]