Covid-19: Health workers 'sick' with fear at thought of second wave
 Worcestershire Acute Hospitals NHS Trust
Worcestershire Acute Hospitals NHS Trust"The levels of anxiety amongst our staff that we may go back to what we saw in April is beyond anything I have ever experienced in over 30 years in the health service."
Dr David Rosser, chief executive of the University Hospitals Birmingham Foundation Trust, was talking to a weekly coronavirus briefing when he described seeing unprecedented levels of concern among his colleagues.
And, although hospitals have outlined a number of measures put in place to support staff, some of those who worked through the first few months of the pandemic have told the BBC they felt worried, panicked and overwhelmed at the thought of facing a second wave.
Sir Patrick Vallance, the government's chief scientific adviser said on Monday the UK could see 50,000 new cases a day by mid-October.
And on Tuesday, Prime Minister Boris Johnson said the UK had reached "a perilous turning point" as he outlined a series of new coronavirus restrictions that he said could last for six months.
We spoke to medical staff to see how they were approaching the possible fresh wave of cases.

'A scary time'
Clementine Stott, an organ donation specialist nurse at Worcester Royal Hospital, was redeployed to the intensive care unit during the first wave which, for her, meant separating from her 10-year-old son for seven weeks.
"With the virus, we had to adapt to a totally different way of working," she said.
"I think any clinician who looked after a Covid patient found the loss of control a terrifying thing because you didn't know how the disease was going to go.
"Patients who were poorly with the virus didn't behave in the way normal ventilated patients would respond to treatment, the normal things didn't work and it was a scary time.
"But there was a lot of camaraderie, we tried to really pull together and look after each other, to go back a second time is depressing and something people will struggle with.
"The one thing in going through that is you think it is a unique situation, it was a bit of a novelty and you were pulled through by the adrenaline of it, facing it for a second time is something else really."
 Getty Images
Getty ImagesA lot of workers would be dreading the "sheer discomfort" of the personal protective equipment (PPE) they have to wear, she added.
"Over a 12-hour shift, it is quite overwhelming," she said.
"When you first get into it all you do get that panicky feeling, which is part stress and partly because you are wearing all of it.
"That alone is quite a challenging thing, it sounds like small thing but day in day out, I know that is something a lot of nurses will be dreading."
But she said hospitals were able, this time, to prepare earlier for a possible rise in cases.
"I know my own hospital trust is definitely making preparations, thinking about capacity, making those decisions in advance rather than in a rush, so that is a positive thing and we know better now how to treat the disease," she said.
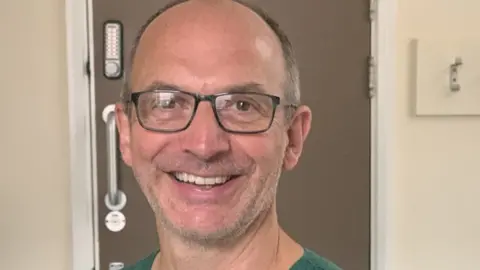 Sandwell and West Birmingham Hospitals NHS Trust
Sandwell and West Birmingham Hospitals NHS TrustDr Nick Sherwood, clinical lead for intensive care for Sandwell and West Birmingham Hospitals NHS Trust, said this year represented the hardest he had ever worked.
During the peak of the virus, he moved into a caravan at the hospital to protect his wife and son.
"The ones it was hardest for were the ones who were not used working in an intensive care unit," he said.
"Nurses whose day job is not dealing with critically ill patients might come in and on their first shift see four patients die.
"Certainly no small number of staff have been emotionally traumatised by it.
"It is something I never thought I would have to do in my career, I like to think I am pretty resilient and tough, but lots of times I would have to go to a quiet place and collapse a bit and then pull myself back together and do it all again.
"Trying to break bad news over the phone was bad enough for us, but I have no idea what it was like for the families.
"The thought that I might have to do that all over again, I am not looking forward to. Not just personally for me and my team, but because I have seen what it was like for patients and their families."
'We'll cope even better'
Charge nurse Terry Ma, who works for the same trust, was off work for six weeks after contracting the virus himself in early March.
When he returned, he was looking after Covid-19 patients in A&E.
"I was still very scared because wasn't sure whether I could actually get the virus again," he said.
"I had got my strength back but I still got tired quite easily and there were so many changes in department in terms how we worked and the layout,
"But after the first couple of hours I was able to tell myself I was in a safe place.
"I believe because our trust, during first wave of the pandemic did so well, we have already had the experience dealing with a surge in cases," he said.
"I believe our trust, our management, all the staff - from the nursing staff, medical staff, the different ambulance staff - are already experienced to deal with it.
"I am still scared if the same happens again, but I think we will be able to cope even better."
 University Hospitals Birmingham
University Hospitals BirminghamNathan Samuels, a regional nurse for young people's healthcare based at Queen Elizabeth Hospital in Birmingham, said: "I think there has still been a degree of apprehension, a tense environment.
"We weren't in the peak as we were in March or April but there was still real awkwardness, or a tense, apprehensive atmosphere certainly.
"And I think that has come from people thinking they can't do it again, they can't face what they went through a few months ago.
"So many things caused major anxiety... from staff becoming ill, worrying about families, the PPE, the guidance, the restrictions, the way it made people feel, how ill people were, having to deal with that, the deaths that were happening.
"They were almost having to be people's families, the emotions they had to carry from people who can't see their relative who is ill, and also that person who can't have any visitors, that is difficult for any compassionate human being.
"When I was working during the first peak, I was going in every day, going on wards where people were confirmed to have it.
"Every single day it was the fear that you could potentially go home and harm your own family."

What are hospitals doing for staff working during the pandemic?
Nationally, the NHS has created a range of support for its staff working to treat people with Covid-19.
It includes specialist bereavement support, access to mental health and wellbeing apps as well as group and one-to-one support.
University Hospitals Birmingham has brought in a number of support services, including a mental health and wellbeing support telephone line, an in-house staff counselling service and health and wellbeing hubs.

Mark Butler, chairman of the West Midlands board for the Royal College of Nursing, said: "Our colleagues in the acute sectors are seeing the numbers increasing.
"There is that fear of facing the second wave because this time you know what is coming, you know how bad it could be.
"You haven't had the opportunity to deal with the quantity of patients that you dealt with initially, the emotion that brings in because, as nurses we aren't automatons, we are incredibly passionate about our job and we go in to work with every intention of doing as much as we can for our patients."
 Sarah Link
Sarah LinkSarah Link, a healthcare assistant at the Queen Elizabeth Hospital, in Birmingham, moved into a caravan six months ago to protect her 84-year-old mother.
She is still living in it and said she was "100% dreading the next wave".
"It has been my job for 17 years, I know I have got do it, but I get up in morning and feel physically sick, I don't want to do it," she said.
"Seeing people being taken into intensive care was awful, people short of breath, people going to the intensive unit and not knowing if they would come back, hearing patients' chances of survival."
Mrs Link said she felt staff "know the situation better" but that had done nothing to reduce her worries about what was to come.
"I just hope it is not as bad as it was," she said.

- SOCIAL DISTANCING: What are the rules now?
- BUBBLES: How do they work and who can be in yours?
- SYMPTOMS: What are they and how to guard against them?
- LOOK-UP TOOL: How many cases in your area?

Follow BBC West Midlands on Facebook, Twitter and Instagram. Send your story ideas to: [email protected]
