‘Exploited’ foreign doctors worry about risk to UK patients
 BBC
BBCDoctors recruited from some of the world's poorest countries to work in UK hospitals say they're being exploited - and believe they're so overworked they fear putting patients' health at risk.
A BBC investigation has found evidence that doctors from Nigeria are being recruited by a British healthcare company and expected to work in private hospitals under conditions not allowed in the National Health Service.
The British Medical Association (BMA) has described the situation as "shocking" and says the sector needs to be brought in line with NHS working practices.
The BBC has spoken to several foreign medics - including a young Nigerian doctor who worked at the private Nuffield Health Leeds Hospital in 2021.
Augustine Enekwechi says his hours were extreme - on-call 24 hours a day for a week at a time - and that he was unable to leave the hospital grounds. He says working there felt like being in "a prison".
The tiredness was so intense, he says, there were times he worried he couldn't properly function.
"I knew that working tired puts the patients at risk and puts myself also at risk, as well for litigation," he says. "I felt powerless… helpless, you know, constant stress and thinking something could go wrong."
Nuffield Health disputes those working hours, saying its doctors are offered regular breaks, time off between shifts, and the ability to swap shifts if needed. The company adds that "the health and wellbeing of patients and hospital team members" is its priority.
Augustine was hired out to the Nuffield Health Leeds Hospital from a private company - NES Healthcare. It specialises in employing doctors from overseas, many from Nigeria, and using them as Resident Medical Officers, or RMOs - live-in doctors found mainly in the private sector.
Augustine says he was so excited to be offered a job that he barely looked at the NES contract. In fact it opted him out of legislation that protects UK workers from excessive working hours - the Working Time Directive - and left him vulnerable to a range of punishing salary deductions.

Listen to File on 4 - Paul Kenyon investigates the 'brain drain' of doctors from developing countries to work in the UK

Augustine is far from alone. The BMA and the front line lobbying group the Doctors' Association has given the BBC's File on 4 and Newsnight exclusive access to the findings of a questionnaire put to 188 Resident Medical Officers. Most of the doctors were employed by NES but some were with other employers.
It found that 92% had been recruited from Africa and most - 81% - were from Nigeria. The majority complained about excessive working hours and unfair salary deductions.
For years now, the World Health Organization (WHO) has warned against the "active recruitment" of doctors and nurses from developing countries with severe shortages of medical personnel. The WHO has compiled a list of 47 such countries - most of them in Africa. The UK government has incorporated that list into its own code of practice - calling it the "red list". In effect, it makes Nigeria a no-go destination for British medical recruiters.
So how did the doctors come to be working in the UK in the first place? We travelled to Nigeria and witnessed another troubling side to this story.
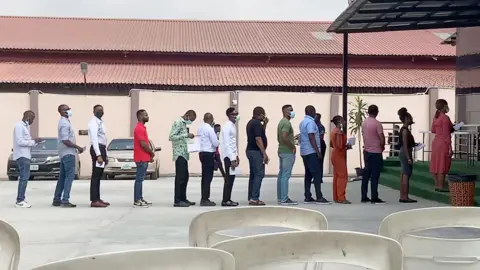
In an exam hall in Lagos, the country's biggest city, we found hundreds of doctors queuing to take what's called a Professional and Linguistic Assessments Board test - or PLAB 1. The paper is set by the General Medical Council in London and is the first step required by the British medical authorities to secure a licence to work in the UK.
The doctors we spoke to said they were attracted by the potential of higher salaries and better working conditions. The event was being overseen by staff from the British Council - an organisation sponsored by the Foreign Office.
The GMC also offers the exams in several other red-list countries - Ghana, Sudan, Pakistan and Bangladesh.
Both the GMC and British Council deny they are involved in "active recruitment" and say they're simply helping provide a service for doctors wanting to come to the UK independently - something that is allowed under the guidelines.
In Augustine's case, he was studying for the second part of those PLAB exams in the UK, when he was approached by NES Healthcare and later offered visa sponsorship and a potential job.
While that does appear to have been "active recruitment" - NES says it wasn't, because it is not a recruitment agency and, as such, only engages with doctors from overseas once they've already committed to practising in the UK. But the Department of Health and Social Care told us the UK code of practice did apply to NES - so the company was in breach of it.
We spoke to several African doctors recruited in this way by NES. They all had similar stories about what the terms and conditions of their contracts meant in reality, once they had been hired out to private UK hospitals.

Dr Femi Johnson was sent to a different hospital to Augustine, but says he was also expected to work 14 to 16-hour days and then be on call overnight. "I was burnt out," he says. "I was tired, I needed sleep. It's not humanly possible to do that every day for seven days."
But when he needed a break because he was too exhausted to continue, NES were entitled to deduct money from his salary. The company says that is to cover the cost of finding a replacement doctor, but Femi says it leaves NES doctors in a terrible dilemma.
"In situations like that, I always make that internal discussion with my inner self - 'Femi are you doing right by yourself and are you doing right by the patient?'" he tells us. "Unfortunately, I haven't always been able to answer that question."

Some NES doctors have received help from Dr Jenny Vaughan from the Doctors' Association. She receives many complaints from Resident Medical Officers and says the UK healthcare system has developed into two tiers - one for NHS doctors, the other for international recruits working in the private sector.
NHS doctors can only be scheduled to work up to 48 hours, and if they request, up to 72 hours a week.
"No doctor in the NHS does more than four nights consecutively because we know that it's frankly not safe," says Dr Vaughan.
"This is a slave-type work with… excess hours, the like of which we thought had been gone 30 years ago.
"It is not acceptable for patients for patient-safety reasons. It is not acceptable for doctors. "

We took our findings to the BMA - and its deputy chair, Emma Runswick. She told us the situation was a "disgrace to UK medicine".
"Our international colleagues have come a long way to the UK, and have found conditions so exploitative it beggars belief."
NES Healthcare told us that our "feedback about doctors' experiences" with the company was "extremely positive". It says it provides doctors "with a safe and supportive route to pursue their career choice in the National Health Service, and in the UK healthcare system more generally, and that their work is of "great benefit to the British public."
