CQC report: Care of people with learning disabilities 'inhumane'
 BBC
BBCToo many hospitals for people with learning disabilities or autism are providing poor care which is, at times, undignified and inhumane, the care regulator for England has said.
The Care Quality Commission (CQC) found physical restraint part of the culture in some places, and cases of patients secluded or segregated for 13 years.
The review was prompted by a BBC News investigation.
Care Minister Helen Whately said the findings were "deeply concerning".
"Nobody should be receiving such poor care," she said.
"We are already taking action, including investment in community services, independent case reviews of people in long term segregation, and the ongoing work overseen by Baroness Hollins.
"I am determined that this level of care should no longer have any place in our health system, and will carefully consider the recommendations in this report."
The CQC said national change was needed to stop people "falling through the gaps".
The NHS said it was reducing the number of people in specialist hospitals.
A spokesman added that, since 2015, the number admitted had been cut by nearly a third and the NHS was committed to reducing that further while it invests more in community support and improves the quality of inpatient care.
The CQC's review was prompted by a BBC File on 4 programme in 2018 which highlighted use of restraints on disabled patients.
Following that report the regulator was commissioned by Health and Social Care Secretary Matt Hancock to look at the use of restraint, seclusion and segregation of autistic people.
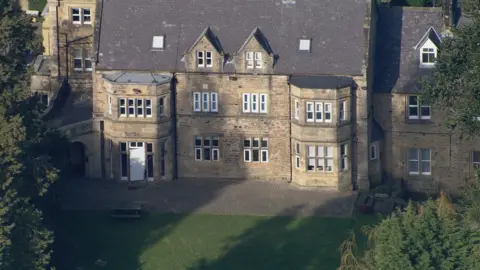
A Panorama programme in 2019 also exposed the mistreatment of residents at Whorlton Hall Hospital.
The specialist hospital in County Durham was closed after undercover filming showed staff intimidating, mocking and restraining patients with learning disabilities or autism.

CQC inspectors visited 43 hospital wards for people with a learning disability or autism, and specialist child and adolescent mental health wards, and other facilities.
They found most of the mental health wards were not therapeutic environments and could be "noisy, chaotic and unpredictable".
People were seen "as a condition or a collection of negative behaviours", the report found, with the result often being restraint, seclusion or segregation.

Bethany's story

The report highlighted the case of Bethany, a girl with autism and extreme anxiety who was kept in seclusion for almost two years.
She was held in what her father Jeremy has described as a "cell" at St Andrew's Healthcare in Northampton, as revealed by BBC File on 4.
Jeremy told the CQC report that her regular staff had no training or understanding of her diagnosis and her behaviour got more challenging, leading to self-harm.
"This anger and self-harm was met by regular restraint, she was held down by multiple people for up to four hours," he said.
Occasionally handcuffs and leg straps were used to contain her as well as "suffocating spit hoods".
Bethany was eventually awarded damages for her treatment after St Andrew's Healthcare, NHS England Walsall Council and Walsall Clinical Commissioning Group accepted her care did not always comply with the mental health practices and "there were unfortunate delays in moving Bethany from what became an unsuitable placement for her".
Her father told the report she was now in a setting which had been created with her input with fully-trained staff.
He said: "The unnecessary medicinal straitjacket has been weaned off and replaced with compassion, understanding and a desire to move Beth to a productive, fulfilling life."

Patients were "often" subject to restrictive practices because they did not receive care early on, it found.
The regulator also said it was concerned that some people were being prosecuted for injuring staff, when a failure to treat their needs may have contributed to their aggression.
The review also found:
- Most (81%) of 313 wards for children and young people had used physical restraint in the previous month
- The length of time people spent in long-term segregation ranged from three days to 13 years
- A lack of suitable care in the community was preventing the discharge of 60% of people it saw during its review
- Some people in seclusion were not allowed to wear their own clothes, while others lacked a clean environment and crockery, cutlery and toilet paper
In one case, ward staff stopped the mother of a 24-year-old in long-term segregation from visiting for five months, prevented the patient from using the toilet on occasion, and left her in pain for months with an injured arm.

Will this report lead to change?

Part of the tragedy that lies behind today's report is that the failings of long-term hospital care for people with learning disabilities and autism are well documented - in abuse scandals, in report after report calling for change and in missed government deadlines for their closure.
But the problems start long before people reach hospital.
I've spoken to family after family who say if there had been enough specialist help when their child's behaviour first became challenging, usually during puberty, then they might not have reached a crisis.
They struggled to get the community support needed to keep their child out of hospital, but local help centred on the individual is likely to cost less than the huge sums paid for inpatient care.
This report underlines the predictability of many of the problems and sets out clear solutions.
The question now is will it lead to change this time.

The CQC found the ward environment, a lack of specialised training and support for staff meant patients' care did not always meet their needs, with people in community-based services experiencing a better quality of life.
The report Out Of Sight - Who Cares? has called for better capacity in the community and across education and health and care to provide earlier care and prevent people being admitted to hospital.
Dr Kevin Cleary, the CQC's deputy chief inspector of hospitals and lead for mental health, said seclusion and restraint should only be used in extreme cases.
"We saw too many examples where people were subject to unnecessary restrictions and examples of people's human rights at risk of being breached."
He added people often ended up in hospital because they "did not have the right support early on" and said that once in hospital people often did not receive specialist treatment and had no support to leave.
"There is no excuse for this," he said.
Edel Harris, chief executive of the learning disability charity Mencap, said the findings were "shocking but sadly not surprising", adding "people deserve to live in homes, not hospitals".
A NHS spokesman said the NHS has funded a restrictive practice programme led by the Royal College of Psychiatrists that had "already resulted in the reduction of physical restraint and seclusion" and said it would be backed by "intensive support for the 20 young people's inpatient services where the use of restraint is most prevalent".
