The puzzle of UK’s half a million missing workers
 BBC
BBCFor the first time, more than 2.5 million people in the UK are out of work because of a long-term health problem. The number has jumped by half a million since the start of the pandemic - but, BBC News analysis reveals, the impact is spread unevenly across the country, with some regions and types of job far more affected.
For Mary Starling, there are good days and bad days.
The 61-year-old is on strong painkillers, for arthritis. She needs a knee replacement - but that could mean another 18 months on an NHS waiting list.
"I feel despair - but I'm resigned to it," she says. "I understand it isn't possible to magic up something, though it's wearing not being able to plan my life."
'Being useful'
Mary, a former nurse who later worked for the World Health Organization, has already had seven knee operations.
She gave up full-time work in 2004 but continued in part-time and voluntary roles until the pain became too much.
Mary is keen to return to that work - but needs her operation first.
"My job was a huge part of my life and I miss it," she says.
"I miss the camaraderie - and I miss being useful, in a sense."
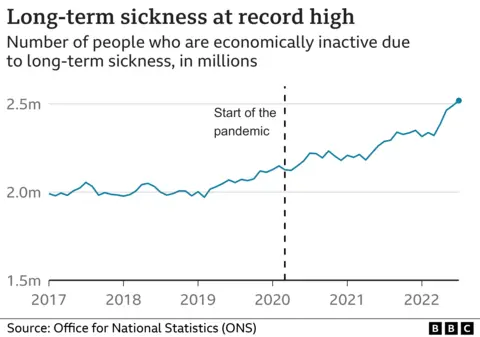
Something strange seems to be affecting the UK workforce.
The country is in its fourth year of sharply rising chronic illness.
The highest rates are among 50- to 64-year-olds - but there have also been significant increases in some younger groups.
Although the link is not conclusive, the Bank of England has said record NHS waiting lists are likely to be playing a "significant role".
And there are hints of this in Office for National Statistics (ONS) data.
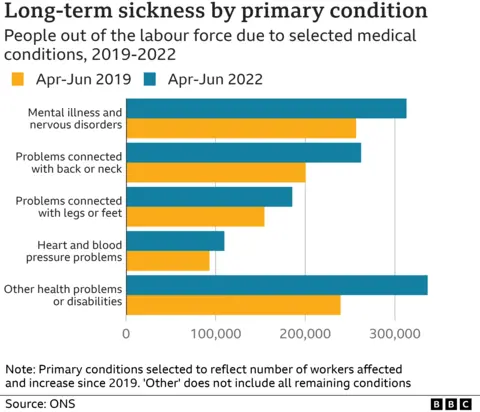
Some of the largest increases are in people reporting mobility difficulties, such as leg and back problems, or heart and blood-pressure problems.
More younger people, in particular, say they are not in work because of different forms of mental illness.
And separate NHS waiting-list data for England paints a similar picture - with lengthy delays for knee and hip replacements, cardiac surgery and community mental-health care.
But the largest increase in long-term sickness is in the catch-all "other health problems" category, likely to include some of those with "long Covid" symptoms.
Patrick Dumayne, a milk-tanker driver by trade, caught the virus in July 2020.
"For a while, I started to recover - and then, I went downhill again rapidly," he says.
As he works out at a gym in Welshpool, Powys, the 54-year-old's breathing is still laboured.
"At the worst point, I was suicidal. I am a 6ft-tall truck driver and biker - and I just sat down at the end of the bed and broke down," Patrick says.
"A big part of that was not being able to work - both the finances and not having that routine every day. It was truly horrible."
Patrick has been receiving support from the Welsh government and now plans to get back behind the wheel early next year.
Both long waiting lists and long Covid are part of the problem, independent charity the Health Foundation says - but as sickness rates began rising a year before the pandemic, they are unlikely to be the main causes.
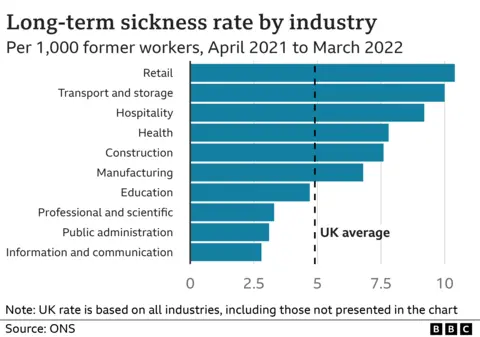
BBC News analysis of ONS Annual Population Survey (APS) data shows large variations in sickness, with high - and rising - rates among people who recently worked in transportation, retail or hospitality.
Jobs requiring more physical effort are more likely to lead to leg, back and other musculoskeletal disorders. While in solitary jobs, loneliness can be a real problem.
Every year, one in four truck drivers experiences mental-health issues, according to the Road Haulage Association.
"It doesn't help that roadside facilities are often poor and when they do find somewhere to pull up for the night, they're faced with unhealthy food choices," the association's Sally Gilson says.
Health inequalities
Workers in lower-paid, manual jobs tend to have poorer health and life expectancy in the first place. The reasons for this are complex, taking in everything from diet and smoking, to access to GPs, to the quality of local housing and green spaces.
The concern - from the Health Foundation and others - is the pandemic might have worsened some of these underlying health inequalities.
BBC News analysis of the latest ONS data, up to June 2022, also reveals stark differences across the country.
The highest long-term sickness rates are in Northern Ireland, north-east England and Wales.
But in London, which has a younger population, the numbers have actually fallen 3% since the start of the pandemic.
The largest rises were in the parts of the Midlands, south-east England and Wales. The East Midlands alone has seen a 21% jump, to a record 176,400 people.
Many of the 50- to 64-year-olds now reporting ill health as the main reason for being off work have already been out of the jobs market for several years for other reasons, such as early retirement or caring responsibilities, Institute of Fiscal Studies (IFS) research suggests.
If that's the case, the impact on the economy from those missing workers may be not as bad as some had feared.
But it still leaves the government with two distinct problems - how to:
- keep those people in a job when many employers desperately need more staff
- deal with a population apparently becoming less healthy in the long term
"This is a serious change," IFS research economist Beatrice Boileau says.
"And any policy that only looks at one of those issues is not going to be successful."
A government review into workforce participation, ordered by Chancellor Jeremy Hunt, is due to report back early next year.
Minister for Disabled People Tom Pursglove said: "It is clear a heathier, more productive workforce is key to driving growth and tackling inactivity.
"Government and employers must work together to unlock talent for those who may be facing health barriers."
You can follow Jim on Twitter.
Data visualisation by Liana Bravo and Nassos Stylianou.
