Deborah James: Her passionate vision for the £6.8m she raised
 Getty Images
Getty ImagesIn the last few weeks of her life Dame Deborah James raised an incredible sum of money - almost £6.8m - for research into new cancer treatments and making sure more people know about the disease.
She was passionate about one area of cancer research in particular - personalised medicine.
Experts say it is "one of the most fundamental breakthroughs in cancer medicine" in recent decades.
It's about giving patients care that is tailor-made or bespoke to their own cancer, rather than using a one-size-fits-all approach to therapy.
Progress in this field is gathering pace, spurred on by advances in genetic testing and a greater understanding of the defences our own bodies mount against cancer.
It doesn't yet work for everyone and still needs refining, but personalised cancer medicine is already giving some people extra years of life.

 Sophie Umhofer
Sophie Umhofer 'From what the doctor said, I should not be alive right now"
One of them is 40-year-old Sophie Umhofer from Warwickshire, who was diagnosed with advanced bowel cancer when she was 36.
When we spoke she had just celebrated her children's birthdays - a huge milestone for her, as she had not expected to be alive to do it. She had even written birthday cards for her children to open in her absence.
She says the chance to have personalised medicine made a huge difference, "allowing her to live again, to be a mum again".
When her aggressive bowel cancer was first diagnosed it had already spread to her liver, and she was given just three years to live at most.
She had conventional treatments - including surgery to remove as much of the tumour as possible, followed by chemotherapy to try to kill remaining cancer cells.
But Sophie says the chemotherapy, which attacks healthy cells too, left her feeling "like an 80-year-old", too tired and weak to be the parent she wanted to be.
Within months she and her family faced the news that it was no longer working.
Sophie's NHS doctor tried a different approach as a last resort - a personalised medicine originally developed to treat skin cancer, which the drug company Bristol Myers Squibbs agreed to provide for free on compassionate grounds.
 Sophie Umhofer
Sophie Umhofer Sophie told me: "From what the doctor said, I should not be alive right now. It was like night and day.
"On chemotherapy I felt like a complete failure as a mum. On weekends I would just drag myself around the house to be near the children and then just end up falling asleep.
"I got to the stage where I questioned the point of being around."
Once she switched to personalised treatment, she says she got her energy back.
"I did have some difficult side-effects. But now I can be a mum again."
Sophie's latest scans show no active cancer. For now she will have regular tests to check she remains free of the disease.
The drugs Sophie took - Ipilimumab and Nivolumab - are a type of immunotherapy. These drugs, which boost or change how the immune system attacks cancer, have proven so successful in her and in some other patients that they have now been approved for use for people across the UK with specific, advanced bowel, kidney and other cancers.

A new way to think about cancer
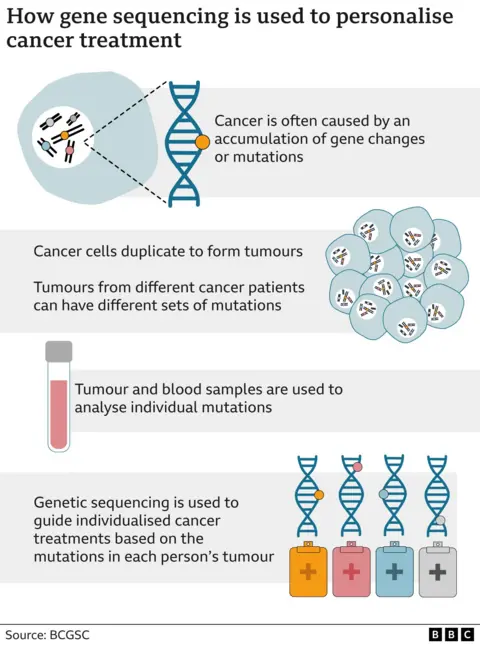
The move towards more personalised treatment is only possible because of a huge shift in the way cancer is understood.
A few decades ago cancer was often thought of as a single disease - with many cancers of the bowel, for example, being treated the same.
Advances in medical technology mean the genetics of individual tumours can be mapped - so-called gene sequencing.
One person's tumour can be genetically very different to someone else's, even if they belong to the same basic type of cancer, such as breast or bowel.
Crucially, these differences influence how individual cancers behave and respond to treatment.
These extra details can guide scientists to find better ways to attack cancers, making new drugs or choosing existing ones that are more carefully targeted to match the way each person's tumours grow and spread.
'Busting cancer's disguise'
For Sophie, genetic tests showed her cancer had a change or mutation called MSI.
The mutation meant the disease was in some ways more obvious to her immune system - our bodies own in-built defence systems - then other tumours can be.
But the problem was it was unable to attack them successfully on its own.
This guided doctors towards a type of personalised treatment called immunotherapy.
It works by boosting the abilities of the body's own immune system to spot, mobilise and destroy cancer.
When it comes to cancer our immune systems can have trouble doing this because tumours find ever more cunning ways to out-smart them.
In Sophie's case, the tumour cells had in-effect tricked her immune system into treating the cancer cells as healthy cells.
One of the immunotherapy drugs she took, Ipilimumab, helped, though a series of steps, to turn on her immune response, allowing special immune cells called T cells to be activated.
The other medicine, Nivolumab, then removed the disguise that the cancer cells had put up to "trick" her immune system.
The activated immune cells were then able to identify the cancer cells and attack them.
 BBC News
BBC News'A cure for some'
Prof Richard Wilson, an expert at Glasgow University and adviser to the charity Bowel Cancer UK, says immunotherapy is one of the greatest success stories of personalised medicine so far.
It is offering up the chance of a cure for a small group of patients who had few options previously.
And for others it helps control the disease, often giving precious extra years of life.
There are a number of different immunotherapies being trialled and refined, with the hope of offering them earlier as treatment, before cancer has a chance to take hold around the body.
Some take a person's own immune cells and "super-charge" them to recognise an individual's own cancer better. The cells are then infused back in to the body to fight.
Prof Wilson says this is one area of research that the money raised by Dame Deborah could go towards.
"We want a wider range of immunotherapies and other targeted treatment to treat and cure a wider range of cancers, and crucially ones with fewer serious side-effects," he said.
'Personalised prevention'
The ultimate hope is delivering personalised care to everyone who needs it, and at every step of their cancer journey.
In an ideal world, this would include personalised early detection and prevention too.
 Getty Images
Getty ImagesOne way to do that, Prof Wilson believes, is to offer genetic testing of cancers to all patients.
At the moment it is only offered in certain circumstances, particularly for people living with advanced disease.
Prof Wilson works for the Experimental Cancer Medicine Centres Network where some tumours being studied go through a panel of 300 gene tests or more - something he would like to see become commonplace.
It is conceivable that in the future this could spur on an era of personalised prevention - where people have their genes mapped to understand what their cancer risks might be.
They could even be given targeted drugs or vaccines to help prevent cancer from developing, he says.
This may only be something scientists dare hope about for now, but other improvements - like advances in surgery, chemotherapy, radiotherapy and imaging - are all helping improve the lives of people with cancer.
For now, the most important things people can do to help reduce their chance of cancer are to lead a healthy lifestyle and watch out for any worrying signs - like a change to their normal bowel habit - so the disease can be avoided or treated as early as possible.
This greater awareness is a huge part of Dame Deborah's legacy.
Prof Wilson says: "What an amazing job she has done, using her illness to help others.
"It is in an incredible gift that she leaves to humanity."
Graphics by Visual Journalism Team

An intimate tribute to Dame Deborah James. Following her death, we hear from friends, colleagues and fellow cancer patients as they celebrate her life and legacy.

