NHS in bleak position as A&E waits worsen, say doctors
 EPA
EPAA&E waits have sunk to their worst levels in England since the four-hour target started, with doctors warning the situation is bleak ahead of winter.
A quarter of patients waited more than four hours for treatment in September - with even longer waits being recorded elsewhere in the UK.
It comes as ministers and GPs clashed over demands that practices see more patients face-to-face.
The government has handed GP practices £250m to take on temporary staff.
But the British Medical Association said they were "hugely dismayed" with the plan, saying it would not solve the problems.
The winter rescue package came on the day NHS England released its latest monthly data for hospital performance.
Lack of access to GPs has been cited as one of the reasons for growing pressures on A&Es.
The A&E performance in England was the worst performance since 2004, when the four-hour target was brought in.
Even greater numbers are waiting over four hours in the other nations with four in 10 patients in Northern Ireland taking over four hours to be seen.
In England, A&E patients who then went on to be admitted to a ward also faced record-long waits for a bed, so-called "trolley waits" - they tend to be the most seriously-ill and frail patients.
Of the 386,000 who were admitted, more than a quarter waited over four hours for a bed to become free. And more than 5,000 had to wait over 12 hours.
Dr Katherine Henderson, of the Royal College of Emergency Medicine, said: "This data is bleak and is a stark warning of the crisis that we are heading towards this winter."
She added that emergency departments were "dangerously" over-crowded and there were widespread reports of ambulances queuing outside hospital because of the demands being placed on the system.
What's in the GP plan?
The £250m funding plan for GPs is part of the extra £5bn Covid fund announced last month to help the NHS through the winter. It comes on top of the £12bn set aside for GP services this year.
Alongside locum doctors - doctors who stand in for others temporarily - GP practices will be able to use the money to recruit other temporary staff such as physios and podiatrists. Pharmacists are also being encouraged to see people with minor illness to relieve the pressure on GPs.

Health Secretary Sajid Javid said the new GP rescue package would help relieve pressure on the whole system.
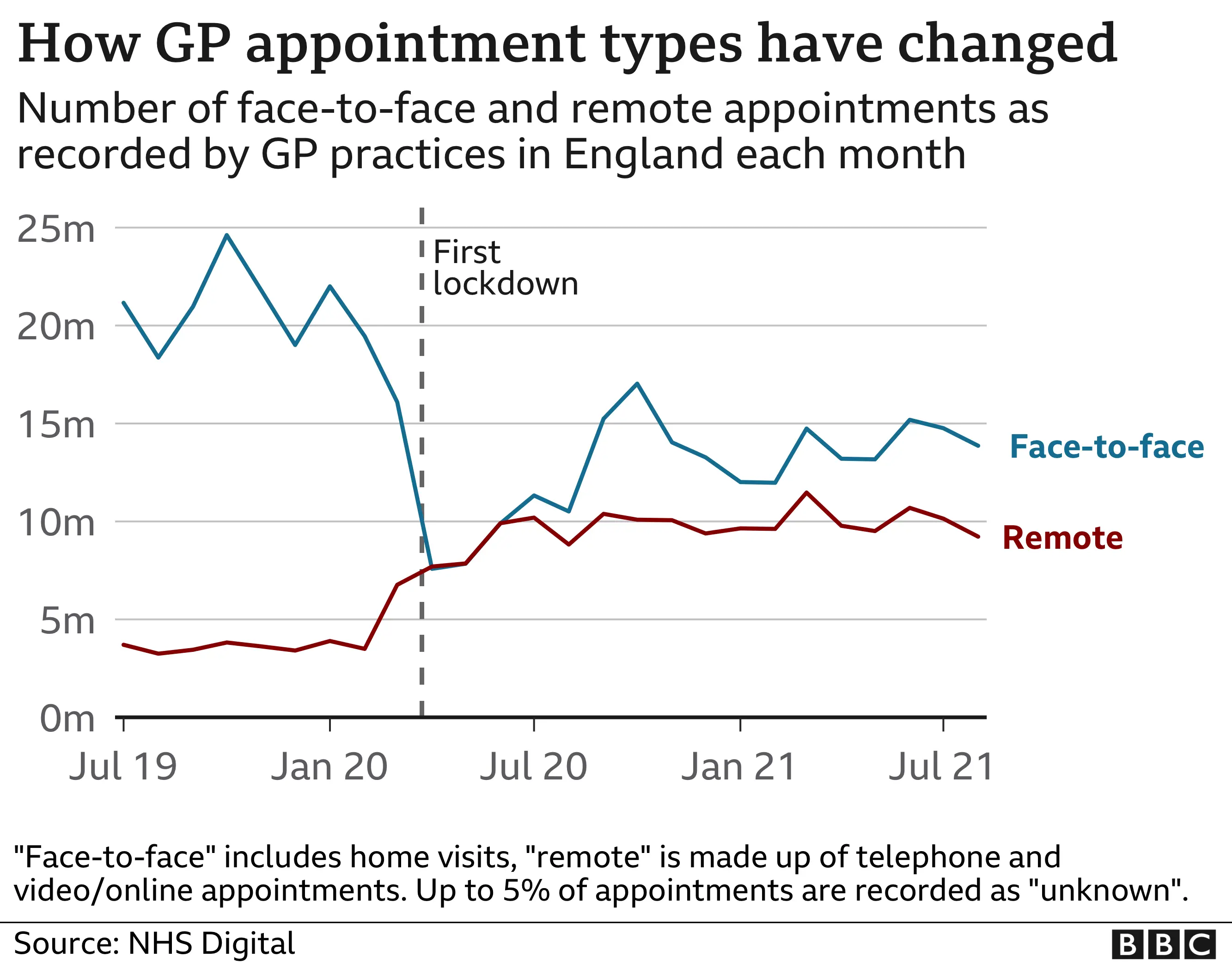
Only 58% of patients were seen face-to-face in August - the first full month following the ending of restrictions.
That compares with 54% in January and more than 80% before the pandemic.
Patients have also complained of long waits on phone lines to book an appointment.

'GP would not see my 84-year-old mother in person'
Kevin Fogarty said his 84-year-old mother was initially refused face-to-face contact with a GP, despite having an infection in her leg following a biopsy.
"She had not been seen for two years. However, an infection developed in the wound but the GP still wouldn't see her. We had to put pressure on them."
Mr Fogarty, 60, said the practice in Somerset eventually agreed to see her in person and she is now getting home visits from a nurse to tend to her wound.
"GPs seem to be the only group not getting back to normal services, while the likes of shop workers and everyone else are getting on with it.
"Telephone and video calls are helpful as an initial consultation, but the GP must see the patient should they insist or there is a requirement."

Alongside the extra money, social distancing rules are also expected to be relaxed in GP surgeries and responsibility for signing fitness-to-work and fitness-to-drive certificates will be able to be passed on to other staff.
Mr Javid said: "I'm determined to ensure patients can see their GP in the way they want, no matter where they live.
"Our new plan provides general practice teams with investment and targeted support. This will tackle underperformance, taking pressure off staff so they can spend more time with patients and increase the number of face-to-face appointments."
GP surgeries will be named in league tables if they are judged to have failed to provide an appropriate level of "access".
But Dr Richard Vautrey, of the British Medical Association, said he was "hugely dismayed" with the package. "It offers very little and shows a government out of touch with the scale of the crisis on the ground."
He said patients would "continue to suffer" and find it harder to book appointments.
"It is disappointing to see there is no end in sight to the preoccupation with face-to-face appointments."
He said in-person appointments were still a key feature of GP care but the pandemic had proven phone or video consultations were "entirely appropriate and appreciated" by many.
The rescue package comes amid the government's ongoing struggle to increase the number of GPs.
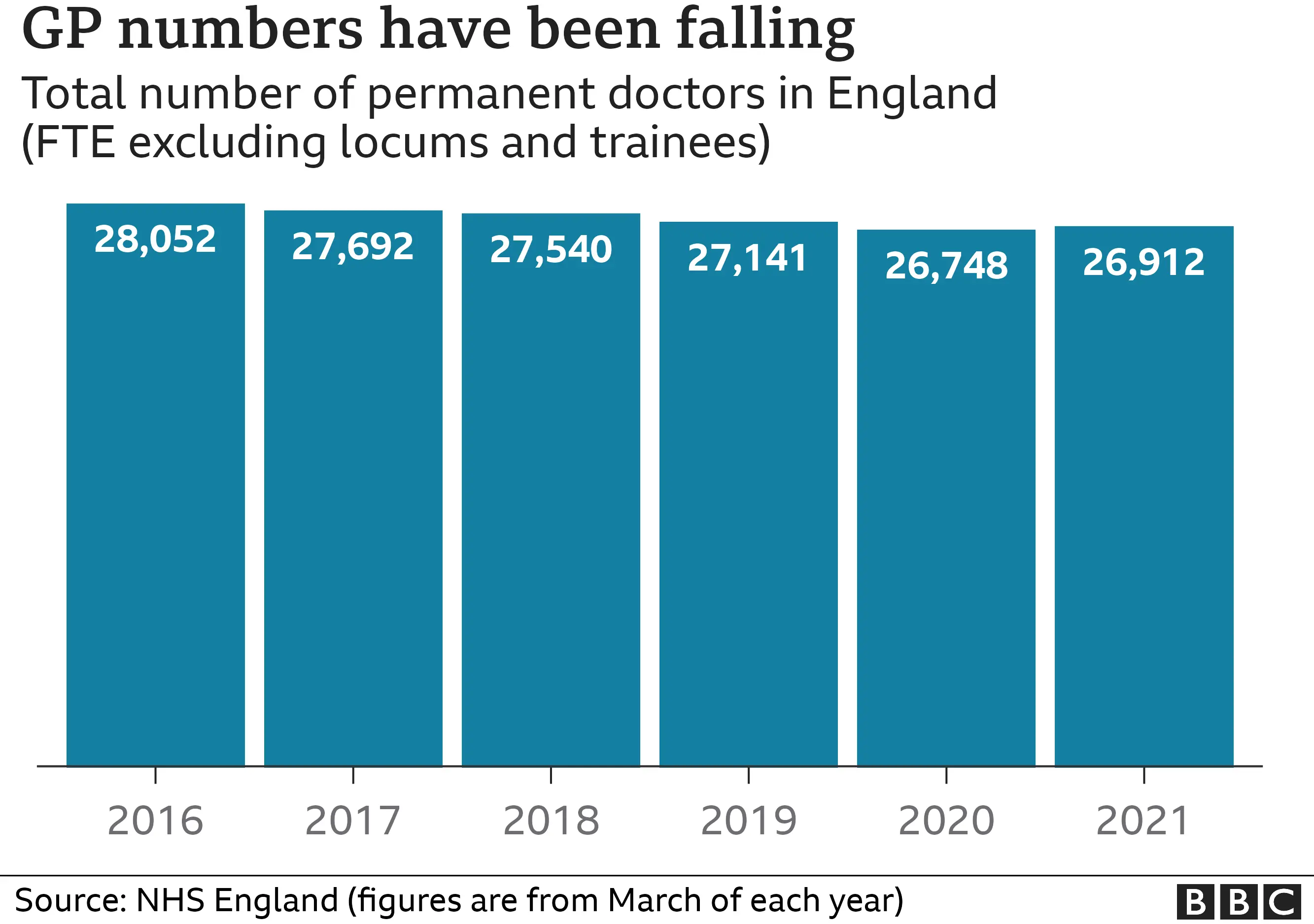

Over the past five years the total - in terms of full-time posts - has fallen despite successive government drives to increase numbers.
NHS Providers, which represents health bosses, said its members were particularly worried about A&Es alongside mental health and cancer services.
Deputy chief executive Saffron Cordery said: "The NHS is fighting fires on multiple fronts as they try to recover care backlogs, increased demand for emergency care, treating patients with Covid and preparing for what is likely to be the most challenging winter yet for the NHS.
"In a matter of weeks, we will face our first winter where both flu and Covid are in circulation."

- THE READER: A clandestine love affair leads to guilt and betrayal
- SEX AND RELATIONSHIPS: How cultural attitudes can shape a marriage

