Coronavirus doctor's diary: 'Our hospital could soon be overwhelmed'
 Getty Images
Getty ImagesA rapid rise in patients acutely ill with Covid-19 is threatening to overwhelm Bradford Royal Infirmary, and other Yorkshire hospitals. Regular diary writer, Dr John Wright, and two consultants from the infirmary describe the pressure on beds and staff.
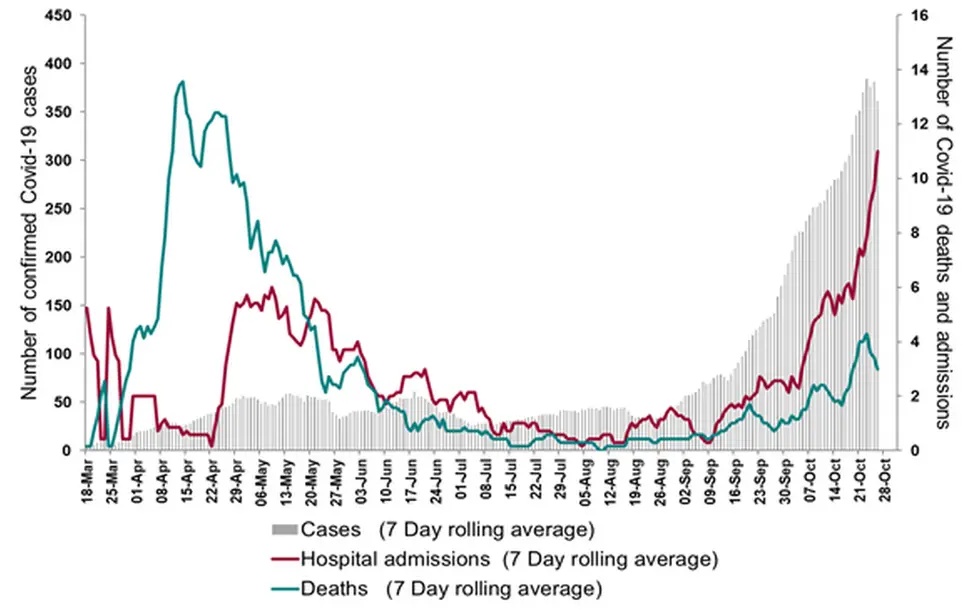
Bonfire night and Halloween have come early in Bradford. The hospital is on fire and things are getting scary as more and more wards are engulfed. As with the first wave in March, the surge in cases came gradually and then suddenly. We have 130 in-patients acutely ill with Covid-19, overtaking our peak at Easter. Fifty patients were admitted in the space of 48 hours. The pressures of finding beds and staff are huge. Over 200 staff are off sick and the school half term has compounded the situation as our clinicians take much-needed breaks or just child-mind at home.
It is all so familiar, and yet at the same time all so different. In March we had emptied out the wards to become a dedicated Covid-19 isolation hospital. This time we have our normal flow of patients admitted with seasonal infections and acute exacerbations of chronic diseases, while also trying to maintain some of our urgent elective surgery.
Covid-19 admissions and deaths at Bradford Royal Infirmary
In March there was a call to arms and all staff rallied around the flag. This time there is a weariness and fatigue. "Groundhog day without the adrenaline," as one of my colleagues described it.
I sympathise with the anti-lockdown advocates. The economic and social damage from the pandemic is going to be catastrophic, and probably outweigh the clinical impact of the virus. However, when you see patients fighting for their lives, drowning in air, it reinforces the primacy of our humanity and compassion. Above all we must care for our patients, protect the NHS from being overwhelmed and speak up to prevent transmission.
Dr Alex Brown, consultant geriatrician

It's getting increasingly busy. We have big problems trying to open wards, especially around staffing them, and staff are tired and fed up with it - people can't see the light at the end of the tunnel.
The other difference this time is that the hospital is busy with other work.
The number of wards we have to go to on our rounds make it feel like a safari ward round - I think I went to about four wards yesterday and it's the same for other colleagues. Some of us are concentrating more on "Red" Covid wards (for infectious patients) and some on the Green (for patients without Covid).
We're struggling to find wards to convert to red and when you come in in the morning it's the first thing you think: has a new ward been converted to be a red ward and how is that being staffed?
Every patient coming in now is being swabbed and we are much better at assessing who has it, but occasionally some people you think don't have it turn up positive and they're sat in your Green bay. So then you have problems assessing whether to isolate other patients round them, isolate those contacts around them. Do we then stop admitting to that area, do we have to have that area deep cleaned, which takes some of your resource out for a while? It's a major problem.
In my ward at the moment, which is meant to be green, we are getting one or two people every week who have no symptoms and turn up positive.

Front-line diary
 Tom Lawton
Tom LawtonProf John Wright, a doctor and epidemiologist, is head of the Bradford Institute for Health Research, and a veteran of cholera, HIV and Ebola epidemics in sub-Saharan Africa. He is writing this diary for BBC News and recording from the hospital wards for BBC Radio.
- Listen to the new series of The NHS Front Line in November on BBC Sounds and the BBC World Service
- Or read the previous online diary entry: 'We blame Eat Out to Help Out for our tragedy'
- Check out all the diary entries on the BBC Radio 4 website

The hospital has cancelled elective surgery but when this started in March time this ward was empty. Now it's full. We will try and turn over as many patients as possible but on Friday morning it will be full. We are running out of resources.
People are very weary of it.
Sometimes I sadly struggle at times to remember who my juniors are. They're all in masks, you see them every day and you're not too sure what their names are - you've lost a lot of that personal touch. It's that which motivates people to feel part of a team, to actually get on and come in every day.
It worries me, the pressure that's being put on the junior doctors at weekends. Whether it's because I've had Covid and have a degree of "long Covid", or just because I'm weary because everyone's weary of Covid, I can't tell. I feel life's a complete routine: work, falling asleep. I have lost energy and can't tell why.
Part of me is worried about catching it again. There aren't many cases of that but you've just got to be careful. I've never been as ill as I was and that was a shock to the system because you think you can bounce back from everything. It was a shock to the system and tells you you have to be careful.
Dr Debbie Horner, consultant in critical care
 John Wright
John WrightBradford had only a few weeks where there was very little Covid. Since early September numbers have started to go up but it's become exponential.
Our starting point is a nearly full hospital anyway so we've increased the number of wards we have open for Covid patients. One of the things I've noticed this time is there are fewer patients needing to go on to a ventilator in intensive care. So there are globally now more patients than we had in hospital at the peak of the first wave but most are out on the wards on oxygen or CPAP (non-invasive ventilation with oxygen).
This means the pressures on the hospital are different but as big and as worrying as they were in the first wave. Modelling shows if we continue on present trends, in three to four weeks we will have filled every bed in the hospital. What do we do after that?
Normally we'd divert A&E to other hospitals, but they're also all full. The only place with critical care beds is Airedale and they have five spare beds. Everywhere else in the region is full.
And the regions adjacent to us are in the same if not a worse position. I'm really worried that if there's not something really significant done to reduce the number of patients getting Covid we're going to be overwhelmed.
I'm very worried. I'm tired and I think everyone is. The nursing staff don't see an end in sight, and once numbers started to go up again in September we saw a lot of sickness among staff. I think what drove it was this awareness that it wasn't over and we were going to be seeing more and more over the winter months.
Follow @docjohnwright and radio producer @SueM1tchell on Twitter

- SOCIAL DISTANCING: Can I give my friends a hug?
- PAY-PACKET SUPPORT: What will I be paid under the new scheme?
- SUPPORT BUBBLES: What are they and who can be in yours?
- FACE MASKS: When do I need to wear one?

