Covid: Is it time we learned to live with the virus?
 Getty Images
Getty ImagesThe constant mantra is the virus must be suppressed and contained. But how do you do this when people can be infectious without knowing they have it? Where it can be passed on silently because people do not develop symptoms?
The nation has been brought to a standstill once at immense cost to the economy, education and health more generally. And now with cases rising, there is the constant threat of more and more restrictions being imposed. But are we fighting a losing battle? Do we instead need to learn to live with the virus?
It's 'utter chaos' now
Prof Carl Heneghan, the head of the Centre for Evidence Based Medicine at Oxford University, says the current situation is "utter chaos" with a constant stream of new restrictions and schools sending whole year groups home when just one person tests positive. All this at a time when the level of infection is still very low.
This, Prof Heneghan says, is the consequence of trying to suppress the virus. Instead, he argues we should accept it is here to stay and try to minimise the risks, while balancing that against the consequences of the actions we take.
In particular, he's concerned the Covid test is actually so sensitive it's picking up what is effectively dead virus as it spots traces of it months after the person has stopped being infectious.
"We need to slow down our thinking. But every time the government sees a rise in cases it seems to panic," he said.
Hospital admissions matter 'not cases'
The argument put forward by Prof Heneghan and a number of other experts is that more weight needs to be put on disease rather than cases. While hospital admissions have started rising they are still incredibly low compared to the spring and the increase is much more gradual than it was.
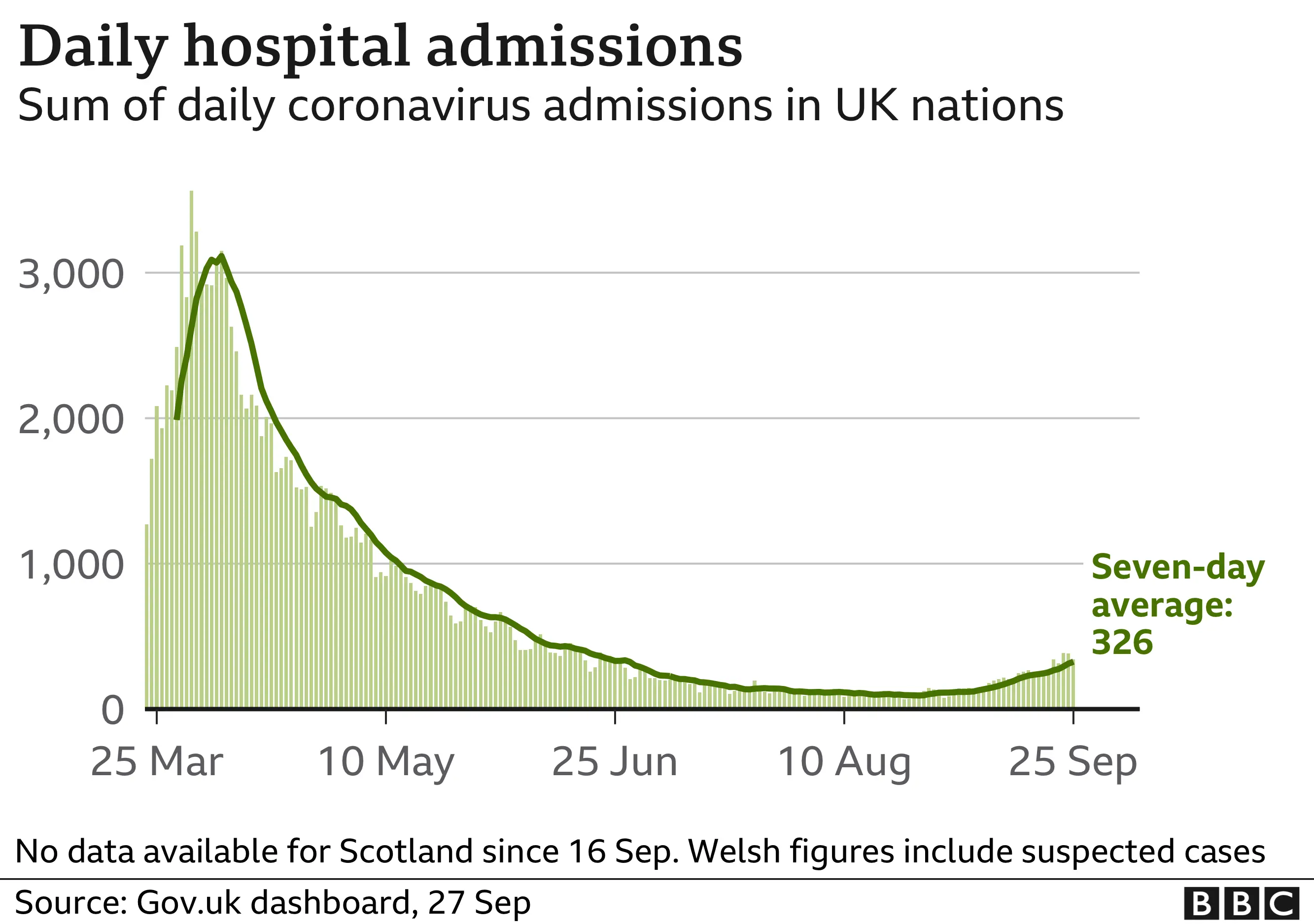

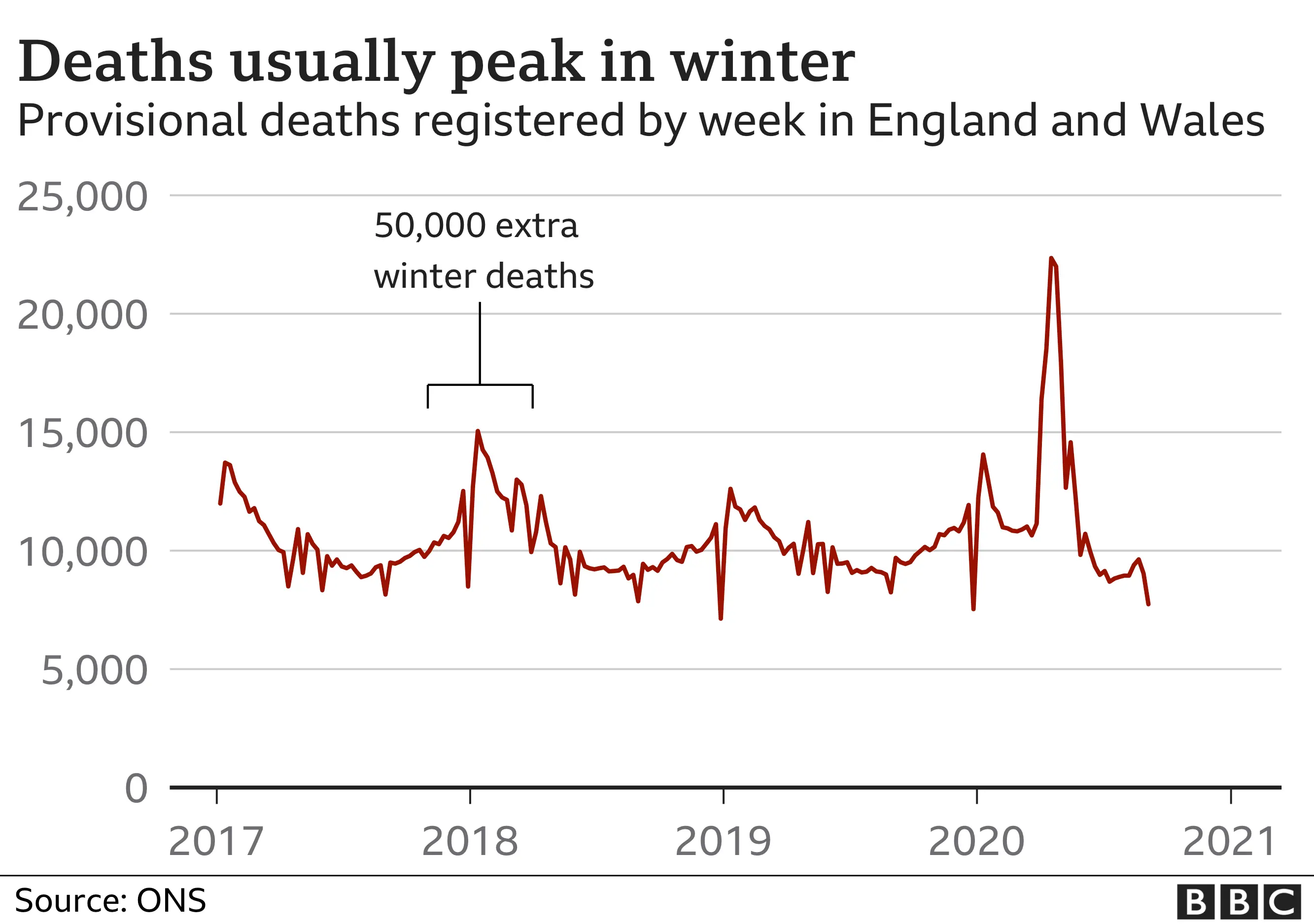
What is more, rising admissions for respiratory illness and, sadly, deaths are what you would expect to happen at this time of year as you head into autumn and winter when these viruses always spread more.
Some years are worse than others. In 2017-18 there were 50,000 extra deaths over winter compared to the rest of the year, mainly because of the cold weather, a virulent strain of flu and an ineffective vaccine.

In fact, Prof Robert Dingwall, a sociologist and an adviser to the government, believes the public may well be now at the stage where it is "comfortable" with the idea that thousands will die from Covid just as they are that they die of flu.
He believes it is only a particular element of the public health and scientific leadership who worry about driving down the infection level and is critical of politicians for not being "brave enough" to be honest with the public that the virus will be around "forever and a day" even with a vaccine.
What's the risk of loosening our grip?
The problem of relying on hospital admissions is that you can find yourself behind the curve. Hospital cases are a result of infections from a few weeks back - so if they spiral out of control more draconian measures may be needed than would have been otherwise.
The other issue, says Prof Christina Pagel, from University College London, is "Long Covid" - the patients who still struggle months after an infection. She says it would be "irresponsible" to allow the virus to spread as it is still less than a year old and we are still not certain of what the long-term risks are.
She also says if infection rates go up in the younger, healthier age groups it will be difficult to keep it from spilling over into more vulnerable ones.
Prof Mark Woolhouse, an expert in infectious disease at Edinburgh University, agrees this is a risk. But he argues the government must carefully "balance the harms" of Covid with the consequences that come from trying to contain it. He says there is already growing evidence the "cure has been worse than the disease" because of the wider societal costs.
The death toll has undoubtedly been terrible. More than 40,000 deaths are linked to Covid. The burden of those have fallen on the very old. The average age of death has been over 80.
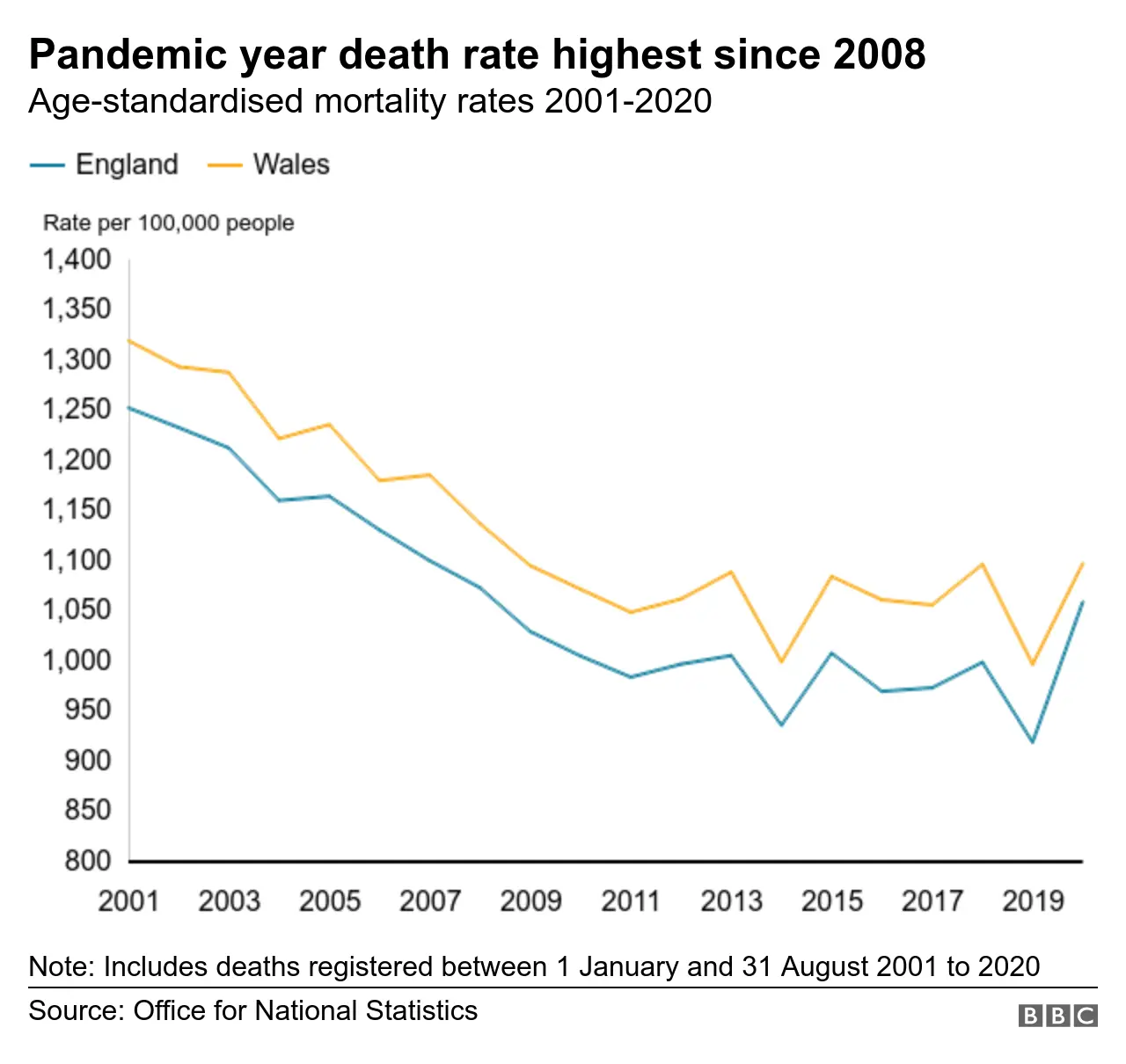

And if you look at the age-adjusted mortality rates, which take into account the size and age of the population, you can see that while 2020 has undoubtedly been a bad year compared to recent years, what has been seen in terms of people dying is not completely out of sync with recent history. It is actually comparable with what happened in the 2000s.
How can the vulnerable be protected?
Prof Woolhouse says lockdown simply deferred the problem, but did have the benefit of buying time, which he thinks could now be used to better protect the vulnerable.
That means intensive targeting of testing at care homes to prevent the virus from getting in - four in 10 deaths have been among care home residents. Similar steps will be taken to protect frail people who receive care in their own homes.
Beyond that Prof Woolhouse says what is needed is a "chain of trust" whereby more care is taken when you have contact with an individual who is at higher risk. That, he says, may mean not seeing them if you think you have been in busy places where you may have been exposed.

- SOCIAL DISTANCING: What are the rules now?
- SUPPORT BUBBLES: What are they and who can be in yours?
- FACE MASKS: When do I need to wear one?
- SCHOOLS: What will happen if children catch coronavirus?

And naturally people in higher risk groups will themselves be taking more precautions than those who are not - something that simply was not happening in February and March until the extent of the spread of the virus was realised.
This should be a consideration, many health experts say, from the age of 50 upwards. But, of course, it should be proportionate with the risk.
While it starts going up at 50, it is still very slim. But it then rises directly with age, which is quite unusual for an infectious disease. Perhaps the easiest way to understand it is to consider it like this - an infection with the virus essentially doubles your risk of death that you face in any given year from injury or illness. The older and more unhealthy you are, the higher the risk on both counts.
The other factor to consider is that doctors are in a much better position to treat severe illness. Two steroid treatments have been found to reduce the risk of death in the seriously ill, while much has been learned about how Covid behaves, which means hospitals will be better prepared for problems such as blood clots and kidney damage.
It means many are confident the scale of deaths seen earlier will not be repeated.
What about herd immunity?
Allowing - or perhaps accepting - some spread also brings us on to perhaps the most contentious point, immunity. There is great hope a vaccine will be developed. But what if it isn't? Or what if it does not trigger a strong enough immune response in the older age groups?
You are then reliant on getting enough younger people vaccinated to create herd immunity. Will they do this for a vaccine that has been produced so quickly to protect them against a virus that is unlikely to cause complications?
 Reuters
ReutersThe other way immunity develops is through exposure. Like other coronaviruses, all the evidence on Covid points to infections giving people some immunity that then wanes, but is followed by re-infections that cause milder illness. Over the years this is likely to lead to coronavirus becoming just another of the seasonal virus we experience every year. Although, as always, that needs to caveated with the fact this is a new virus so scientists are learning more about it all the time.
That process could take years, even decades some think. But others are more optimistic. Prof Sunetra Gupta, of Oxford University, believes there may well be more immunity already than we think because of a combination of natural immunity and more exposure than screening suggests - she says the antibody markers that are relied on to identify previous exposure are not so reliable for this particular virus.
She says allowing young and healthy people to be exposed over the winter will be of benefit in the years to come. "This is how we have always managed viruses. Why is this so different? If we keep introducing restrictions and lockdowns while we wait for a vaccine it will be the young that suffer the most, particularly those from more deprived backgrounds. We can't keep doing this - it would be an injustice."
Follow Nick on Twitter

