Caroline Wyatt: The fight to reverse damage caused by MS
 BBC
BBC"I don't like to think of the future. It's such a big question mark. I just keep living in the present."
Karine Mather was diagnosed with MS when she was 27, although she noticed the first symptoms much earlier.
It started off as a mental-health issue with anxiety and depression, she remembers. Later, she noticed she was starting to limp when she walked longer distances.
Karine began using a walker to help with her balance and stamina, and then a scooter when she could no longer walk very far.
"I got to the stage where the wheelchair became quite liberating, and gave me back a sense of freedom again. Now I rely on the power-chair full-time because I can't stand by myself any more."

Now Karine and her wife, Sarah, have had to give up their full-time jobs.
Karine was forced to stop working as a customer service adviser at a bank because she could no longer fulfil the physical demands of work and Sarah gave up working as a data analyst so she could take care of Karine.
Now 34, Karine retains the use of just one hand, and suffers pain, stiffness and spasticity in her body that has got worse as the disease has progressed.
"It feels like a fist clenching all the time. And I have days when my mind is cloudy and I miss out words and sentences."
Both remain upbeat but the financial, as well as the emotional, impact of MS has been huge.
Karine's MS is the type known as "primary progressive", or PPMS, which meant that for the first years after diagnosis, no disease-modifying treatment was available.
One new drug - Ocrevus, or ocrelizumab - was recently licensed for early PPMS in the UK but came too late to help Karine.
Now the MS Society is launching an ambitious "Stop MS" appeal, aiming to raise £100m to fund research over the next decade into treatments that can stop the progression of disability in MS.
Since being diagnosed with MS in 2015, after many years of symptoms, I've been looking for anything that might help slow or even stop the progression of my MS, which affects the nerves in my brain and spinal cord.
I last wrote about my MS after travelling to Mexico for an autologous stem cell transplant (aHSCT) in 2017.
Sadly, despite initial improvements, I'm now back to where I was before: slowly but surely getting worse.
The only improvements that have endured are the lifting of some of the crushing brain fog I had before HSCT and less hesitation in my speech.
For both, I am eternally grateful, as they mean I can continue to work at the BBC, in the job I love.
However, I have no idea how long this reprieve will last.
The fatigue that had long been my worst symptom is now back with a vengeance, so that staying awake throughout a busy working day remains a challenge.
That MS fatigue did lift for a few months, and it felt miraculous. I awoke every day refreshed. But then it returned, and I awake after eight full hours fast asleep feeling as if I haven't been to bed at all.
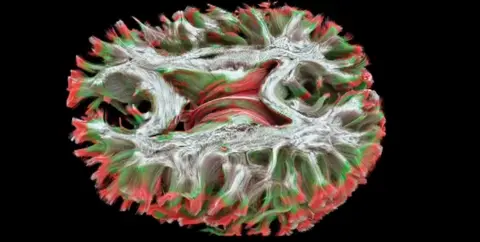 Cardiff University
Cardiff UniversityThe ageing process - including menopause - has almost certainly been a factor in the worsening of some symptoms.
Ageing cells repair less well, and with my faulty immune system apparently determined to keep stripping away the myelin sheath that should protect my nerves, I'm less able now to repair the damage than I was when the disease first began to affect me in around 1992.
Since 2016, I've had to walk using a stick to aid my balance. It is sparkly-topped; an effort to make the accoutrements of disability just a little more cheery.
Dizziness is now a constant companion. It rarely goes away, making car travel or even buses a nightmare. Just turning my head too fast can make me stagger or fall over.
And for the past year or two, my right foot has begun to drag along the ground thanks to foot drop, meaning that I trip more often because I can't fully raise it.
I am always grateful to the strangers who kindly stop to help me up from the uneven pavement when I do fall.
Perhaps most worrying for me is that my right hand no longer works as it used to, catching on the computer keyboard as my outer fingers drag lazily along the keys, sullenly refusing my brain's command to lift.
In the mornings, both my hands and my feet are numb and frozen, then painfully full of pins and needles before warming up enough to be usable a few hours later.
When I wake, I wonder how long it might be until these hands and feet barely function at all, and quickly push that unwelcome thought away.
I'm well aware how very lucky I am that the progression of my MS has been relatively slow - at least until recently. I've learned how better to conserve energy for the things that really matter, though I still chafe at how little I manage to achieve.
Having enough energy to cook a meal from scratch on a day off is a cause for rejoicing. I'm still learning how to save up enough energy for family and friends, and not use up all of my much-depleted ration for work or research.
I have had to face the fact that I have now probably gone from the relapsing-remitting phase of MS (for which a dozen or so treatments exist) into the secondary progressive phase, for which there is currently no treatment licensed in the UK to stop the relentless progression that will affect so many of the 100,000 or more of us living with MS here.
But that may be about to change.
Anna Williams, professor of regenerative neurology at the University of Edinburgh, is looking at how the brain responds to MS damage and how the fatty myelin sheath under attack in MS can be restored more efficiently.

"We have to look at ways to stop the nerves dying," she says. "We want to be able to try to limit that either by keeping the nerves alive, or keeping them working better."
Repurposing existing drugs to help with remyelination should prove the quickest route to therapies for progressive forms of MS, because creating and licensing new ones is a much lengthier and more expensive process.
Prof Williams still sees patients at the Anne Rowling Clinic of Regenerative Neurology in Edinburgh, named in memory of the Harry Potter author J K Rowling's mother, who had MS. (The author this year donated £15m for research at the unit.)
"At the moment, with PPMS or SPMS, we can always give relief for pain or stiffness but we won't change the course of the disease.
"So for those patients, to slow or stop or reverse the disease can only be done with more research, and money is critical for research."
The biggest trial yet in the UK for patients with secondary progressive MS is the MS STAT2 trial, conducted by Prof Jeremy Chataway for the UCL Queen Square Institute of Neurology in London.
The trial is still recruiting at 30 centres across the UK to look at whether simvastatin, a drug used to treat high cholesterol, can slow or stop disability progression. If so, it has the potential to become one of the first disease-modifying therapies for people with secondary progressive MS.

And perhaps most encouraging of all, Prof Robin Franklin and his team at the Wellcome-MRC Cambridge Stem Cell Institute recently published research suggesting a common diabetes drug - metformin - could hold the key to stopping disease progression in MS.
Costing just a few pence per tablet, metformin appears to have an ability to restore cells to a younger, healthier state and encourage myelin regrowth.
The next question is whether it works in people as well as it does in the lab.
Prof Franklin says: "This is a drug that's well tolerated and widely available. There is every reason to believe that the effects that we have seen - which have been so spectacular - will translate into humans.
"This is the great frontier of MS therapy. We're good at stopping the inflammation in MS. What we're not so good at doing is repairing the damage. All this work has given us some real hope that this medicine will reverse the damage done by MS."
I certainly feel rather more hopeful than I did.
I've changed as much about my lifestyle as I can - prioritising sleep, eating healthily, largely giving up alcohol, doing yoga and stretching every day, and cutting back on stress, be that reporting from war zones or attending too many BBC meetings.
But I'm all too aware that time is against me as my ageing brain and body struggle to repair the damage done in their lengthy continuing battle with my own immune system.
My hope now is that these trials will show good enough results in the next few years for at least one or two of the drugs to be rapidly approved for MS so they can help people like Karine and me before it's too late.
I ask Karine what she makes of the current research.
She is suitably succinct.
"I'm sitting here with just the one limb working and I'm thinking - quicker, please."