The 'dual stigma' of alcohol-related brain damage
 BBC
BBCAlcohol-related brain damage, a condition similar to dementia, is poorly understood and often missed by health professionals, a study by charity Alcohol Change UK says.
And patients struggling with the "double stigma" of brain impairment and alcohol addiction often end up in accident and emergency units because of a lack of community services.
The condition affects balance and makes it difficult for patients to process new information. They can also become confused and experience memory loss.
At its most basic, the injury is caused by damage to brain cells from alcohol, which causes them to shrink and die or deprives them of vital vitamins.
Heavy drinking
A man who drinks more than 50 units of alcohol a week, or a woman drinking more than 35 units, for five years or more is at risk of the disease, Alcohol Change says.
"You're talking about a condition that's the result of long-term heavy drinking, which a lot of people are going to say, 'Well someone's done that themselves, it's his own fault,'" Andrew Misell, from Alcohol Change UK, said.
"And then you're talking about a condition which makes someone's behaviour difficult to manage - people can be aggressive, inappropriate, confused and confusing to others"
Last year, the alcohol care team at the Royal Liverpool Hospital treated 79 patients with alcohol-related brain disease.
Patients are asked to sit a test used to diagnose dementia, which has been adapted for this condition.
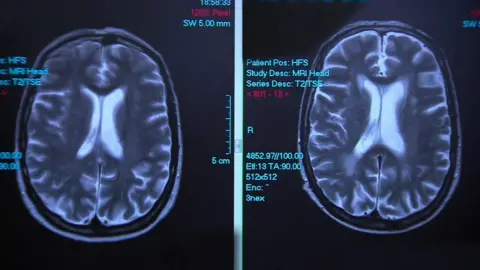
A low score can lead to scans to see if the patient's alcohol intake has shrunk their brain.

If it has, an occupational therapist is then brought in to find out how the brain damage has affected that person's daily life.
"I can assess them getting washed and dressed, cooking some basic food, look at road safety awareness, their ability to manage finances," senior occupational therapist Jenna Simons said.
"If we do a kitchen assessment and they're cooking, and the doorbell rings, they might forget about the cooking and go back to watching TV, so that's then a fire risk."
'Two glasses of wine became a bottle'
Mark Jones, 55, who was diagnosed last November, had been a functioning alcoholic for years but his alcohol intake had become problematic about four years ago.
"I've always enjoyed a glass of wine," he said, "but the glass became two glasses, two glasses became a bottle and it was maybe one and a half, two bottles of wine a day."
By the time he came in to hospital, his short term memory had deteriorated, he had lost his balance and needed a walking frame to move around - all a consequence of his alcohol intake.
Most rehab centres don't accept people with an alcohol-related brain injury.
But the team at the Royal Liverpool managed to find Mr Jones a place at the Merseycare NHS Foundation Trust in the city, which treats people who've had traumatic brain injuries, where he has received help for his short-term memory loss.
"While I don't believe I will get it fully back 100%, it has improved an awful lot since I've been in here," he said.
For his continuing rehabilitation, however, Mr Jones, who is due to be discharged in the next few days, will have to rely on his family - as there are no community services geared up to support his brain injury.
Mr Misell said: "One thing we are very clear about is that, unlike other forms of dementia, such as Alzheimer's disease for example, the progress of the condition is not inevitable," says Andrew Misell.
"It can be reversed. And people can be taught, in a sense, to recover themselves, to re-learn things they've forgotten how to do."
