English 'short-changed on care funding'
 Getty Images
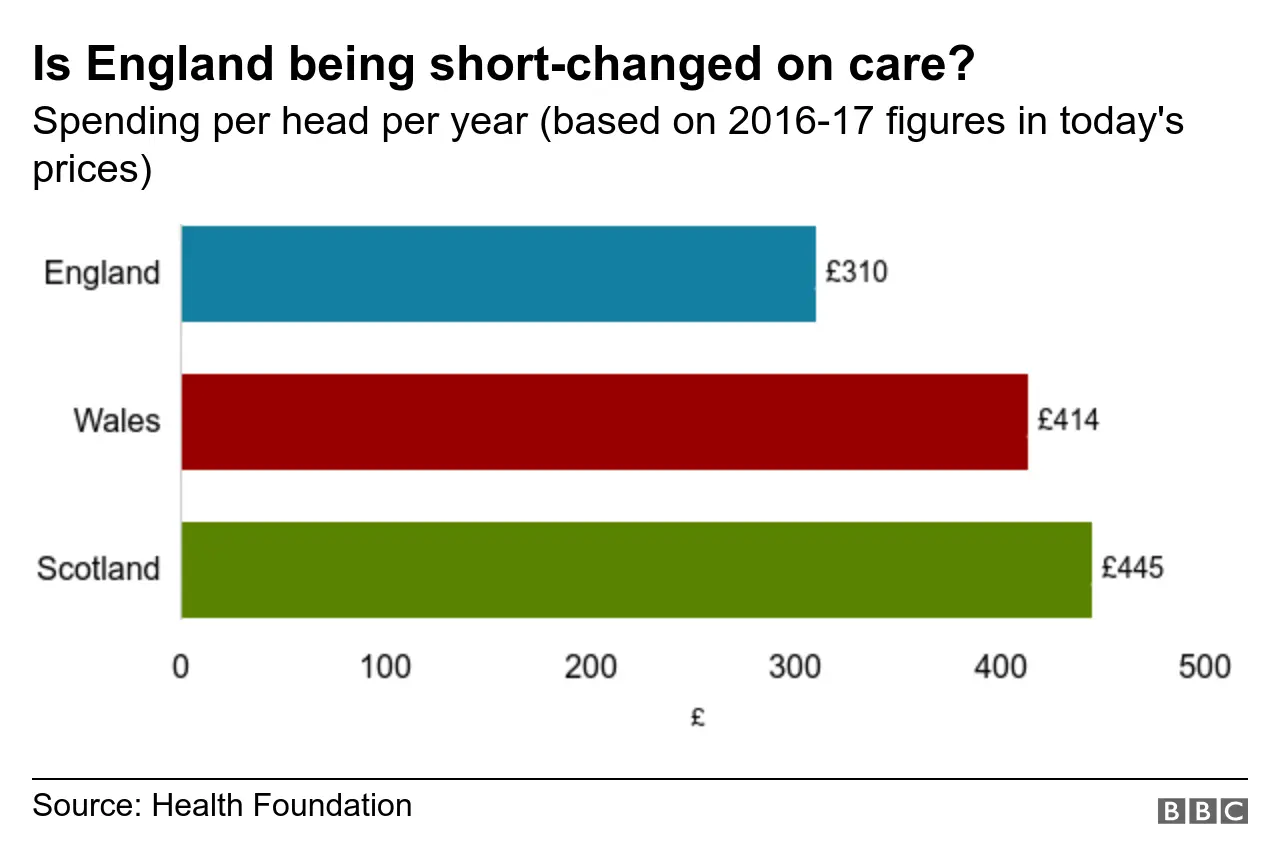
Getty ImagesPublic spending on care for the elderly and disabled is much higher in Scotland and Wales than England, figures show.
In England, £310 per person is spent each year on services such as care homes and home help for daily tasks such as washing and dressing.
But in Scotland, £445 is spent - 43% more than in England - and in Wales it is £414 - 33% more.
The analysis has been produced by the Health Foundation using official spending and population data.
The think-tank said the differences were "huge" and had a major impact on the care that could be provided by councils to these vulnerable groups.
It comes after the BBC revealed a number of councils are at risk of running out of their reserves if current spending continues.
Care spending is likely to be a significant factor in this given it accounts for more than half of local authority budgets.
Ministers in England have promised that new plans for care, including funding, will be published soon.

How the system is failing the vulnerable
Social affairs correspondent Alison Holt
Over ten months, a Panorama team and I saw for ourselves the dilemmas that social care staff in Somerset were facing almost daily - as they juggled the increasing need for help from people who are older or disabled alongside the county council's severe financial pressures.
At the heart of the difficult decisions they were having to make were people, such as 37-year-old Martine. She has severe arthritis and her husband David was exhausted from caring for her and their triplet sons, day and night.
Or Paul, who had learning disabilities. His family had to fight for a place at a specialist residential home, which cost more than the council felt able to pay.
And then there was Barbara, bewildered by dementia, whose daughter viewed the day centre she attended as a life line. It closed because of council cuts. They were offered alternatives, but they lost something that worked.
The pressures we saw are not unique to Somerset, they are being faced across the country as our population ages.
Two things were particularly striking. The first was how hard people were working to plug the gaps in a system buckling under the strain.
The second was the cruelty of seeing families, often at a time of crisis, being confronted by a care system that is confusing, hard to navigate and where few really know what they will have to pay to get the support they need.
Watch BBC Panorama Care in Crisis: Who cares? Wednesday 29 May at 9pm on BBC One

How significant are the differences?

Public spending per head tends to be higher in other parts of the UK than it is in England.
Economies of scale and the rural nature of Wales and Scotland are key drivers for this.
But the analysis suggests what is happening with care spending far outstrips this.
For example, health spending in Scotland is just 8% a year more than it is in England - five times less than the difference in care funding.
Anita Charlesworth, from the Health Foundation, said: "While there are differences in the populations and needs of the UK countries, this cannot possibly account for the huge differences in per head spending on publicly-funded social care.
"Considering the scale of the problem in England, it is perhaps unsurprising that the long-delayed social care green paper is still 'forthcoming'.
"One reason governments have struggled is that any solution is expensive. But transformation is now, more than ever, needed to make the social care system fair and sustainable in the future."
The analysis shows spending per head fell by a tenth once inflation was taken into account between 2010-11 and 2016-17 in England.
If funding levels had grown in line with demand, councils would be spending in excess of £23bn a year rather than the £17bn put aside, the think-tank said.
Over the six-year period spending had also fallen in Scotland and Wales, although not by as much.
What does the extra funding allow Wales and Scotland to do?
In all parts of the UK, care is means-tested with people expected to contribute towards the cost of their care.
But since devolution, differences have emerged in approaches to care.
In England, anyone with assets of over £23,250 has to pay the full cost of their care.
But in Scotland personal care, such as help washing and dressing, is provided free to everyone assessed as being entitled to care.
Meanwhile, in Wales the cost of help in the home is capped, currently at £90 a week.
The point at which individuals are liable for the full cost of all other services is also higher than the £23,250 threshold.
It means the amount people pay for care is likely to be higher in England - particularly for older people who are more likely to have built up assets than younger disabled people.
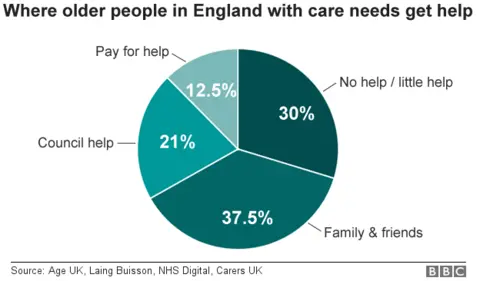
The cost of care is one of the major factors behind why increasing numbers of people struggle without the support they need, Age UK says.
It estimates there are around 1.4 million over 65s who get no care or not enough care.
Councillor Ian Hudspeth, of the Local Government Association, said the system was at "breaking point".
"More and more people are increasingly unable to get the quality and reliable care and support which enables them to live more fulfilling and independent lives."
He added it was "absolutely vital" the government took action.
Ministers in England has been promising a green paper will be published setting out its plans to reform social care since the 2017 general election.
A number of options are understood to have been discussed including a dedicated social care tax on the over 40s and asking for some kind of contribution for those with significant assets, such as property, in return for greater universal entitlement to support.
But the publication of the green paper has been delayed on numerous occasions as ministers have focussed their attentions on Brexit.
The Department of Health and Social Care said the plans would be published at the "earliest opportunity" and pointed out a national recruitment campaign to encourage people to apply for jobs in the care sector had already started.