Parents' care can help premature babies in hospital, says study
 Getty Images
Getty ImagesLetting parents get directly involved with the care of their premature babies in intensive care can help the health and wellbeing of both, a study says.
A trial in Australia, New Zealand and Canada showed babies whose parents took part put on more weight and continued to be breastfed more often than those cared for only by hospital staff.
Parents who participated in the trial also had less stress and anxiety.
The study took place across 26 neonatal intensive care units, with 14 providing the Family Integrated Care (FICare) programme, covering 895 babies born at 33 weeks or before, and the other 12 giving standard care to 891.
Clinical decisions
Parents were involved in:
- bathing
- feeding
- nappy changing
- dressing
- giving oral medication
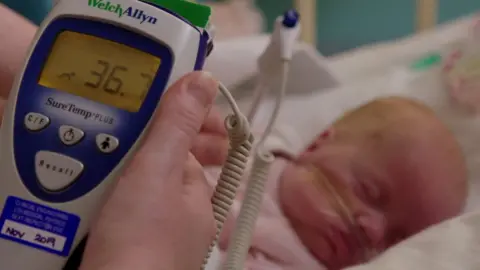
- taking their child's temperature
They were encouraged to take part in clinical decisions and ward rounds and to chart their baby's growth and progress.
And they were kept informed about tasks they could not do, such as adjusting oxygen levels.
Participating parents also had to commit to being at their infant's bedside for at least six hours a day, five days a week and to attend education sessions for at least three weeks.
After 21 days, infants in the FICare group had put on more weight and showed higher average daily weight gain than those receiving normal care.
Their parents also had lower levels of stress and mothers were more likely to breastfeed regularly - six or more feeds a day - than those in the non-parental care group.
Dr Karel O'Brien, from Toronto's Sinai Health System, who was one of the study's authors, said: "How care is provided to the family, not just the infant, has a positive effect on the wellbeing of both infant and family.
"Parents are too often perceived as visitors to the intensive care unit.
"Our findings challenge this approach and show the benefits to both infants and their families of incorporating parents as key members of the infant's health care team, and helping parents to assume the role of primary caregiver as soon as possible."
The report's authors did note that the time commitment required of the parents may have biased the selection of participants.
And Dr Chris Gale, of Chelsea and Westminster Hospital, said the beneficial effects highlighted by the trial were "important" but "need to be interpreted cautiously in light of the risk of bias inherent in the trial".

'I am much more confident in myself as a parent'
Amy gave birth to twins at the Mount Sinai Hospital in Toronto after 23 weeks.
"Family integrated care was a major role in my children's care plan," she says.
"Our experience was and is amazing. We are actively a part of our children's basic care needs.
"I had to give up my job to be here. We live about three hours from Mount Sinai hospital. My husband works during the week and commutes on the weekends to be with us.
"I absolutely felt more of a bond with our children. It's hard to say what their outcome would have been had we not been as active in their care as we have been.
"I believe it would have been a longer road for them and it would have been harder to bond with our babies.
"I am much more confident in myself as a parent. The doctors and nurses listen when I express a concern and they were able to treat infections before they became serious, because I was able to speak up."

Caroline Lee-Davey, chief executive of the premature and sick baby charity Bliss, told the BBC: "This new research adds to the multitude of evidence which shows that enabling parents to take an active role in their baby's care significantly improves outcomes for babies born premature or sick.
"It highlights the need for parents to be supported to spend as much time as they want with their baby in hospital.
"Neonatal units across the country must be properly funded to provide sufficient overnight accommodation and financial support."
'Up and running'
A FICare system has been operating at St James's University Hospital in Leeds since May 2015 and was introduced at its sister hospital, Leeds General Infirmary, last September.
And Dr Liz McKechnie, consultant neonatologist at Leeds Teaching Hospitals Trust, told the BBC that more were springing up around the UK.
"It's up and running in Glasgow, Swansea, Imperial in London and Bradford, and more people want to implement it," she said.
"A huge part of it is empowering the parents and giving them the confidence and information they need so they can manage their babies better.
"From an economic point of view, it's a really good model of care.
"Once the baby is discharged, families seem to need to go to the GP less - presumably because having more time with their babies has made them understand them better."
