Stress, burnout and hope: NHS workers speak out
 BBC
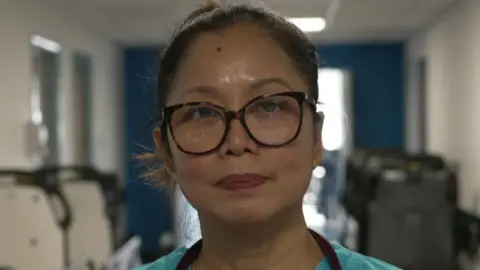
BBC"You have moments when you're human and feel overwhelmed. My way of coping is to take a deep breath, and if I have a chance, go for a 30-second break outside, come back in, then smile again."
Cielito Canejo is a specialist respiratory practitioner. Like many of her NHS colleagues in London, she experiences times of pressure and stress at work. The Covid-19 pandemic caused her to reflect more on her mental well-being.
"The silver lining of the pandemic was that it raised awareness of mental health. For me personally, I no longer felt there was a stigma around it."
While the pandemic is long over, the pressures on the NHS remain. Ms Canejo says she worries about the mental health of her colleagues across the sector.
The latest NHS Staff Survey, published on 13 March, has ranked London as the second worst region in England for morale and burnout (behind the East of England) - with a third of the capital's health workers saying they "often or always" feel burnt out because of the job.
London also scored worst in the category of "work pressure", with three quarters saying they experienced unrealistic time pressures in their job.
Across the NHS, millions of workdays are lost each year due to mental health issues with workload, psychological distress and the pandemic's impact being blamed.
"We worked through the pandemic, serving the nation, and we've had no recovery," says Dr Chaand Nagpaul, a north London GP.
"And since then, we've had to deal with the biggest backlog of care in the NHS.
"The number of patients needing to be seen far outweighs our capacity. This is a recipe for creating stress and burnout."
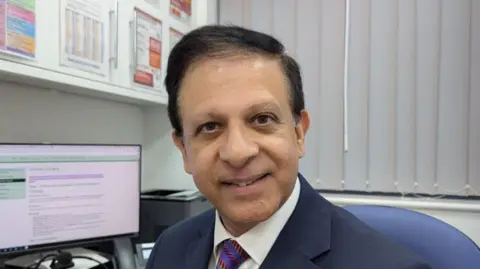
He says his GP surgery is in an area with one of the lowest doctor-to-patient ratios in the country.
Dr Nagpaul adds that the capital has pockets of deprivation where health issues are more common.
In addition, he says, compared with some other parts of the country, London GPs need more time, in order to provide care for patients who may have English as a second language and for asylum-seekers who may need more help with experiences of trauma.
Dr Nagpaul co-chairs the charity Doctors in Distress. It offers support groups and this year is holding an urgent fundraising appeal to help meet demand.
Within the NHS, various services are offered to try to help staff with their mental health.
For example, London North West University Healthcare NHS Trust runs an in-house psychology service and offers on-site exercise sessions. It also brings support directly to staff in the form of a tea trolley.
"We go around with a 'well-being trolley'", says Aderemi Shoyebo, "bringing teas and coffees to staff who otherwise might not get a chance for a break.
"We use it as an opportunity to find out if there's anything they need help with and signpost them to support services."
'Toll on wellbeing'
For Ms Canejo, what helped was journalling, and becoming a mental health first aid instructor. Through helping others' mental well-being, she found it rewarding to her own.
An NHS London spokesperson said NHS staff were working "incredibly hard to meet rising demand and care for more patients than ever before, and we know this can take a toll on wellbeing".
"While there is more to do, the NHS is fully committed to ensuring staff get the support they need, and the health service is now offering more flexible working options than ever before, as well as a range of mental health support available for staff, including access to coaching and wellbeing resources."
A Department of Health and Social Care spokesperson added: "NHS staff have been overworked for years.
"Through our Plan for Change we are turning the NHS around and giving staff the tools they need to deliver the best possible care to patients."
Listen to the best of BBC Radio London on Sounds and follow BBC London on Facebook, X and Instagram. Send your story ideas to [email protected]
