'Health hubs for women would benefit everyone'
 BBC
BBCDedicated women's health hubs should be introduced in Northern Ireland, according to England's Women's Health Ambassador.
These hubs are currently being rolled out across England as part of its Women's Health Strategy launched in 2022.
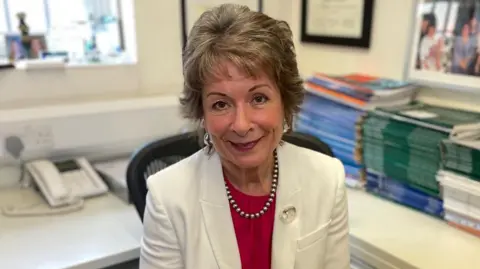
Dame Lesley Regan said these “one-stop shops”, which allow access to care including gynaecology and menopause services, reduced hospital admissions, are cost effective and allow women to get on with their lives.
The Department of Health said it is developing a women's health action plan that "outline the actions" that can be taken in the next three years to improve outcomes for women.
Speaking to BBC News NI, Dame Lesley said making it easy for women to access services prevented "an enormous amount of disease from developing" and “women becoming seriously ill”.

BBC News NI spoke with clinicians and patients at a hub in Tower Hamlets, London.
Dame Lesley, who has been at the forefront of the hub model, said women’s health is fundamental to society.
“When you get it right for women, everybody else benefits and that is a fact, so when you get things rights for women you get happier families and the whole of society benefits,” she said.
'Gave me my health back'

Kate Minns was experiencing several gynaecological issues which were affecting her home and work life.
She said having somewhere that prioritised her health needs helped a lot and travelling to the hub wasn't an issue.
"To have it dealt with very quickly and professionally just gave me my health back basically, which is everything," she said.
Kate was seen by a menopause specialist within weeks of seeking an appointment.
Hormone Replacement Therapy (HRT) and counselling were provided under one roof.
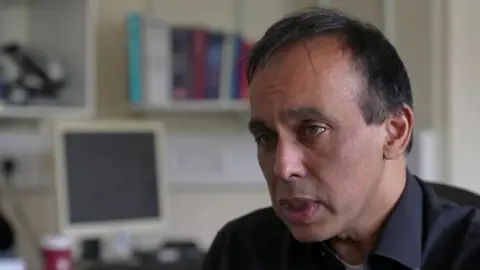
Consultant Rehan Khan said while setting up the hub was a hard sell, waiting list figures prove it is worthwhile and they are starting to "win the battle".
"What really hits home, is when we talk to individual women - they are telling us that no one has listened to them for so long," said Dr Kahn.
"They are telling us that they are so glad that they could get care quickly and they are telling us that they'll come back."
As well as reducing waiting lists, the hub aims to reduce the number of women referred to hospital.
In the old system, GP referrals to specialist clinics resulted in advice for 15% of their patients and hospital appointments for 85%.
The latest picture reveals advice for 34% of patients, 38% triaged to community-based Women’s Health Hub clinics and 26% triaged to hospital-based gynaecology clinics.
The economic case
A 2024 report by the NHS Confederation, Create Health Foundation and London Economics makes the economic case for investing in women's health services.
It argues an additional £1 invested in obstetrics and gynaecology services per woman in England could generate an estimated £319m return to the economy.
Absenteeism from work due to heavy and painful periods, endometriosis, fibroids, and ovarian cysts costs the UK economy nearly £11bn every year.
Around 60,000 women in the UK are unable to work because of the impact of menopause symptoms on their overall physical and mental health.
If those women were to enter employment, earning the average wage of a woman of menopausal age, this could generate an increase in direct economic impact of £1.5bn per year, the analysis suggests.
Dame Lesley said she would argue Northern Ireland can’t afford not to have these hubs.
"They are so cost effective in solving so many problems and stopping them at an early stage, which prevents them becoming more complex and costing even more money,” she said.

The Derry Well Women Centre is involved in a survey asking women about their health needs.
The survey, which will help shape future services, is supported by Queen's University, the Royal College of Midwives and the Department of Health.
Board member, Dr Sandra McNeill, said women often make numerous visits to various health professionals, but a one-stop shop could make diagnosis quicker and save money.
"We can wrap our services around women without spending additional money - it is about realigning the services with the money we have," she said.
Dr Janet Barter is a menopause specialist and lead at Tower Hamlets Women’s Health Hub.
She said patients and clinicians would not accept Northern Ireland's gynaecology hospital waiting lists, which are the worst in the UK.
"It must be very distressing for the women who have to wait and for the doctors and the nurses," she said.
Women can have a scan and a biopsy all on the same day at the Tower Hamlet hub and can return to speak to someone about their results – within 12 hours.
Dr Barter said to make that possible, the health service needs to train a workforce – GPs, hospital doctors and physiotherapists in advance so services are up and running in the future.
In a statement, the Department of Health said the women's health action plan it is developing will highlight the policy and service initiatives "in progress" and outline actions "that can be delivered within current resources over the next three years to improve health services and outcomes for women".
It said the women's health hub at Daisy Hill Hospital and services at the Causeway Hospital's Meadows Unit are examples of health trusts' focus on gynaecology and early pregnancy services.
It said regional structures in trusts and the upcoming action plan should help enhance and develop services through to 2025 "subject to available staff capacity and resources".
