Mental health nurses on 999 calls reduce ED admissions
 BBC
BBCA new pilot project that sees mental health nurses speaking on 999 calls has seen a 40% reduction in the number of people in mental health crisis being admitted to emergency departments (EDs).
The project in the South Eastern Health Trust area, funded by the Public Health Agency (PHA), sees 12 mental health practitioners from the trust work with the Northern Ireland Ambulance Service (NIAS) in its control room in Belfast at the weekends.
It is aimed at people who call 999 in mental health distress.
In the scheme, a medical health practitioner will give a mental health assessment to de-escalate people from attending EDs, and prevent ambulances from going to people that are in mental health crisis.
The trust's project lead, Stephanie Patten, said the pilot has been proving successful so far.
"From April to September, there were 190 [mental health] calls," she told BBC News NI.
"40% of those calls were de-escalated which meant they did not require an emergency ambulance."
Ms Patten said this means people "have the right care and the right response at the right time" when they are in crisis, and don't have to wait on an ambulance or in a busy ED.
"An emergency department is not an appropriate place for someone who is depressed, anxious or distressed to be sitting waiting," she added.
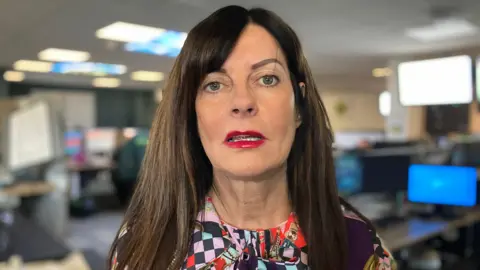
Anne-Marie Scott, one of the mental health nurse practitioners who answers the 999 calls of patients, said most callers are known to them, with some presenting with thoughts of suicide or self-harm and often in great distress.
"We listen to what they say," she said.
"We give them time to vent and then try, with them, to rationalise how they are feeling and try to break everything down.
"Then we can, with their consent, refer on to statutory or voluntary services for additional support."
How does the scheme work?
The project operates on Friday and Saturday between the hours of 19:00 and 03:00, and on Sunday between 15:00 and 23:00.
If a person in the South Eastern Trust area calls 999 in a mental health crisis, they will be transferred to a mental health nurse practitioner to complete a mental health assessment.
An onward referral to a voluntary or statutory service will then be made if it is appropriate.
This prevents patients having to wait on an ambulance or attend a busy ED.
"In these antisocial hours, the patients that are not involved with the mental health team, they have nobody to turn to," Ms Scott said.
Those in a mental health crisis rely on emergency services to go to an emergency department, Ms Scott added, but as they are busy, some patients may be waiting hours to be seen by the mental health team.
NIAS consultant paramedic Karl Bloomer said it is between those times when the "peak" demand occurs.
"We've seen an increase in our demand for mental health calls, and quite often 999 ambulance response, and ED isn't the most appropriate or best care for this patient cohort," he said.
Mr Bloomer said the service has seen a number of benefits from the pilot so far, including properly targeting emergency ambulance responses.

There is another unintentional benefit of the pilot too.
"Our control room colleagues also get support from the mental health practitioners when they have a difficult mental health presenting call," Mr Bloomer added.
"They can lend their expertise to reassure, encourage and educate our staff, so that is a benefit we did not anticipate initially."
While the project is based within the South Eastern Health Trust, with the rollout of Encompass - a digital-based health records system - mental health nurse practitioners have access to Belfast Trust patients and so have been able to widen their reach.
It is hoped in the future it could be expanded further.
"Ideally we would love to see the service rolled out seven days a week and regionally," said Mr Bloomer.
