Extreme pressure at old hospital in Covid - doctor
 Hywel Dda health board
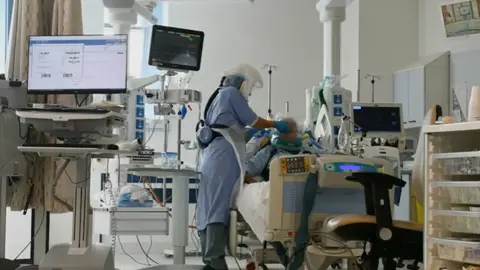
Hywel Dda health boardA senior doctor has painted a picture of the big challenges fighting Covid in Wales' oldest hospital and the stresses on staff during the pandemic.
Prof Philip Kloer told the UK Covid inquiry intensive care in Glangwili hospital in Carmarthen was braced for 192 critically-ill patients, but had only 11 beds,
While the 65-year-old hospital faced less demand than feared and maintained one-to-one critical nursing care, staff had to be "incredibly creative" to create space and work safely.
Prof Kloer, chief executive of Hywel Dda health board, said it managed to redeploy 600 staff to acute hospital care and recruit another 1,100 - including from retail and hospitality - to provide support roles.
Prof Kloer, a former medical director and also a respiratory doctor, said the hospital was opened in 1959 and had a lack of side rooms, very poor ventilation and no air conditioning.
To meet Covid safety guidelines around bed spacing, would have meant losing 113 out of 388 beds at the hospital.
But they created partition walls to help separate patients.
Although the nursing ratio was one to 24 patients on general wards, there were support staff in place for "wrap around" care.
Another 113 beds were provided at a field hospital at a local leisure centre and bowling alley "which looked and felt exactly like a hospital."
But he acknowledged staff were working under extreme pressure.
Prof Kloer said experiences documented in a staff survey in 2021 "were very difficult to read".
It found there had been anxiety over the working environment, with some having sandwiches in their cars during breaks and one reporting crying in a cupboard under the stairs.
There was a shortage of toilet facilities, rest rooms and other staff facilities at Glangwili.
He admitted that there may have also been issues around communication about how to access the stock of personal protective equipment (PPE) after a member of staff complained about being "told off" for ordering visors.
Prof Kloer said to his knowledge, although there were challenges in the summer of 2020, PPE stocks never fell below a two-week supply.
But he admitted with a surge they could have run out and there was "significant concern" for staff.
What was Covid like in Carmarthenshire?
- There were 494 deaths due to Covid-19 in 2020 and 2021 in Carmarthenshire
- The county was in the lowest 25 local authorities across England and Wales for Covid mortality rates during the first wave and below the Welsh average in all but two weeks at the end of May
- But the second wave in early 2021 brought a spike and the peak of the pandemic in Carmarthenshire
- The map above shows the impact of Covid as it moved through different communities, with one area of Llanelli having one of the highest mortality rates in Wales, while it was also high around Ammanford and Llandybie
- Carmarthenshire's Covid infection rate was running above the Welsh average in December 2020, when the country went again into a lockdown
- Subsequent waves peaked slightly lower than the Welsh average, while the vaccination programme meant far fewer deaths
- Hospital admissions with Covid peaked in January 2021, when there were 287 patients across the Hywel Dda health board area
- There have been around 3,500 hospital-acquired Covid infections in Hywel Dda to date. At Glangwili, Prof Kloer said there were "significant challenges" but a"meticulous approach" to outbreaks, including enhanced cleaning and a high focus on PPE, had seen them reduce during the pandemic
'Almost impossible scenario'

The early pandemic estimate was that Glangwilii might have faced the need to accommodate 192 intensive care patients.
But it only had 11 beds and staffing for a potential 16, while Prof Kloer said it was only offered a supply of a third of the ventilators that might have been needed.
He said it was an "almost impossible scenario" to contemplate but the worst case did not materialise.
Prof Kloer said much earlier awareness of the impact on vulnerable groups was an important lesson from the pandemic.
Later, Dr Andrew Goodall, then NHS Wales chief executive, told the inquiry that by mid-March 2020, the health service was anticipating a huge shortage of beds – if scientific modelling on pandemic numbers played out.
He said Wales was facing a shortage of nearly 6,000 hospital beds and almost 1,450 intensive care beds if fears were confirmed.
As well as the modelling, it was “tying in visibly with the images we were seeing, particularly of Italy and Spain, how the virus would spread very, very quickly and have an impact on capacity.”
Health boards were then asked for daily reports on the bed position in their hospitals.
