'Personalised cancer programme gives me control'
 NIKKI FOX/BBC
NIKKI FOX/BBCWhen Julia Beeden discovered she had breast cancer, it was devastating and unexpected.
But the 41-year-old from Cambridge was enrolled in a research programme that analysed her DNA like a barcode and meant her treatment could be tailored to her, giving her "control" to make the best decisions for her future.
Over the past few years, it has emerged that there are many different types of breast cancer, and each one responds in varying ways, so treatment is not "one size fits all".
The Personalised Breast Cancer Programme is operating at five sites across England, the latest being the Norfolk and Norwich University Hospital.
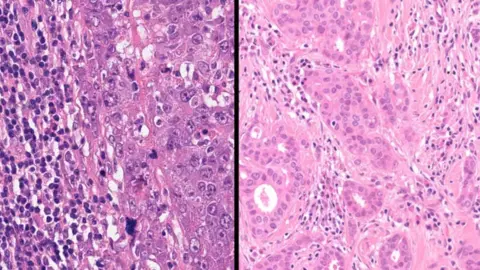 PRECISION BREAST CANCER INSTITUTE, CAMBRIDGE
PRECISION BREAST CANCER INSTITUTE, CAMBRIDGEMs Beeden is one of more than 1,500 women diagnosed with breast cancer, who have had their DNA screened so far.
In June 2023, she found a pea-sized lump under her armpit. She couldn't feel anything in her breast, but the tissue within it was firm and dense and was found to be a tumour that had already spread.
Ms Beeden was placed on the programme at Addenbrooke's Hospital in Cambridgeshire.
She underwent whole genome sequencing (WGS) which analyses the complete genetic code, or DNA of an individual.
It found that her BRCA2 gene, present in everyone, had a genetic mutation, which determined the type of breast cancer she had.
According to some research papers, scientists believe there are as many as 11 different types of breast cancer, although there is some disagreement over the figure as discoveries are ongoing.
 NIKKI FOX/BBC
NIKKI FOX/BBCAfter having chemotherapy and radiotherapy, Ms Beeden was placed on a specific drug for her type of cancer, which she is responding well to.
"One of them is specifically targeted to the fact I have the BRCA gene mutation, and that’s a relatively recent cancer advancement. But I wouldn’t be eligible for that drug unless we knew I had that mutation," she explained.
"I'm not having horrific side effects, so for me that’s a real benefit. Some of the [chemotherapy] drugs I’m on now, I don’t think they existed five years ago.
"The more specialised to you, they are... the more you feel a bit more reassurance that the doctor’s chosen your medication accordingly.
"I would be on a very different set of drugs if I didn’t have that result, and those drugs might not be as effective in reducing my recurrence of cancer, and that’s what it’s all about, minimising my risk for the future so I can carry on with my life."
 JULIA BEEDEN
JULIA BEEDENThe BRCA gene is a gene that helps the body to fight cancer, but having a mutation means it doesn’t function as well, so those with it cannot fight cancer in the same way.
According to studies, the risk of developing breast cancer with a BRCA2 mutation increases from 12.5% to 69%, the risk of ovarian cancer rises from 2% to 17%, and the risk of prostate cancer increases from 12.5% to 41%.
Knowing she had the BRCA 2 gene mutation also meant that by the time Ms Beeden needed surgery, both she and her surgeon had all the information they needed to discuss the best option.
She chose to have preventative surgery on her other breast.
"It was because of that genetic knowledge, that they were able to advise me.
"Angelia Jolie hasn’t had cancer, but she’s chosen to have her ovaries removed for that reason, so she doesn’t struggle with ovarian cancer like her mother did. You can make those choices.
"Knowledge is power, isn’t it? To make a decision about your life."
Ms Beeden said making quick but informed decisions about her treatment meant she was able to get back to her life.
"It's definitely a new normal, but it's as close as I could get," she said.
"At the beginning of the cancer journey, you lose control of everything. I knew they were going to take my hair, everything was going to change - my freedom, my ability to play with the kids next door because of the risk of germs, I couldn't swim - so you literally have to take back control wherever you can.
"I think every element where you feel you've had some information... it gave me that control to make those decisions.
"I hated looking at my choices, and I hated making the decision, but it was my decision and that’s really important."
 NIKKI FOX/BBC
NIKKI FOX/BBCEvery year, around 5,700 women, as well as a small number of men, are diagnosed with breast cancer in the East of England, while around 1,100 women in the region die from the disease.
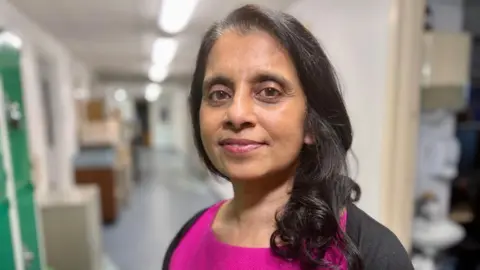
Professor Jean Abraham, director of the Precision Breast Cancer Institute in Cambridge, funded by Cancer Research UK, said that 25 to 30 years ago, breast cancer was a single label, but now it was clear that it was a "very mixed bag" of different cancers.
"Different [breast cancer] sub-types have different natural histories and will come back quicker or slower. So really understanding the genetics behind these cancers really helps us understand how different they are from each other, and how important it is to treat them differently."
The programme is currently running at five sites: Addenbrooke's Hospital in Cambridge, Oxford, Colchester, Ipswich, and now Norwich, where it hopes to help hundreds more women and some men.
"I think it will save the NHS money as we won’t give treatments that aren’t effective and cause toxicity. We can speed up people’s time in hospital and, actually, in the end, we hope it’ll effect how well they do overall in terms of surviving their cancer," said Prof Abraham.
Dr Clare Hannon, programme lead at the Norfolk and Norwich University Hospital, said, for patients who are eligible: "The DNA will be analysed from the same routine biopsy and blood tests, meaning that there are no more tests or appointments than usual and no delays in starting treatment."
 FAMILY HANDOUT
FAMILY HANDOUTMs Beeden's father and mother have subsequently been tested, and the BRCA2 gene mutation originates from the male side of her family. Both her father and grandfather had prostate cancer, but at the time, neither knew it was because of the mutation.
She now hopes her brother, from Bristol, can be tested, so that he would know if he has an increased risk of cancer.
Ms Beeden said that she believed everyone with cancer should be eligible for genetic screening.
"If I had known my risk of cancer when my dad was diagnosed with prostate cancer, I’d have caught it [breast cancer] when it was just a pea sized lump, instead of the tumour getting much bigger and spreading.
"I think it’s something that I and others would always fight for."
Follow East of England news on X, Instagram and Facebook: BBC Beds, Herts & Bucks, BBC Cambridgeshire, BBC Essex, BBC Norfolk, BBC Northamptonshire or BBC Suffolk.
