Why is mpox spreading more rapidly?

 Getty Images
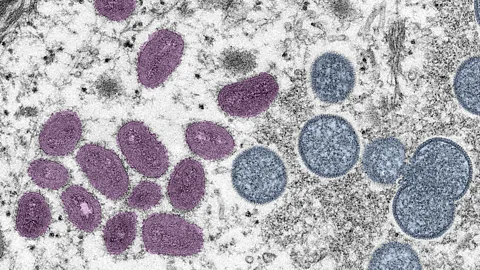
Getty ImagesThe virus that causes mpox, formerly known as monkeypox, was first discovered at the end of the 1950s, but there are signs it has undergone changes in the past three to four years that have enabled it to pass between humans more easily.
The first thing everyone should know about the disease that used to known as monkeypox is that it actually has very little to do with monkeys.
"It was first discovered in monkeys in a laboratory setting in Denmark, it does infect monkeys, and has been isolated from monkeys, but they're not the primary reservoir for the disease," says Sagan Friant, an anthropologist at Pennsylvania State University in the United States. "We think of a reservoir as an animal that can transmit the disease but does not suffer or die from it."
Friant has been studying monkeypox in Nigeria for more than 15 years and was about to begin a new research project just as the Covid-19 pandemic hit. She says it's likely – but not yet proven – that the monkeypox virus originates in rodents. At the end of 2022, the World Health Organization (WHO) announced it was renaming the virus as mpox.
"For a long time, scientists thought that diseases in primates were the most threatening to humans because of our close similarity genetically, and that's true," she says. "But we're realising that infectious diseases from rodents and bats are of increasing importance when we're thinking about spill-over of new diseases into human populations."
Infections that pass from animals to humans are known as zoonotic diseases. Some of these also have the ability to pass from human to human once they make the jump across species.
In that respect, mpox has some similarities to Covid-19. But it's been around a lot longer than the coronavirus behind the recent pandemic. Recent outbreaks of the disease have alarmed global health officials, however, due to the speed at which is spreading. In August 2024, the Africa Centres for Disease Control and Prevention (Africa CDC) declared a public health emergency over a new variant of mpox that is behind a growing number of cases and deaths in several countries including the Democratic Republic of Congo, Burundi, the Central African Republic and Rwanda. A few days later the WHO declared the surge in mpox constitutes a public health emergency of international concern.
Where did mpox come from?
Monkeypox was first identified in 1958 at a laboratory in Copenhagen, Demark when it was discovered in monkeys that had been imported from Singapore a couple of months earlier. The first case in humans was not reported until 1970 when a nine-month-old boy admitted to a hospital in the Democratic Republic of Congo was found to have been infected with the virus. Although the young patient lived in an area of tropical rainforest populated by monkeys, doctors were not able to establish if he had recently come into contact with an infected monkey or if it had come from another source. The boy recovered from the infection, but sadly contracted measles a few days later and died.
 Getty Images
Getty ImagesWhile it is likely there were human cases before this where the virus was not identified – it causes lesions that are similar to those seen in other pox infections such as smallpox – there have since been cases in a number of African countries before the first outbreak in the US in 2003 when 70 cases were reported. It is thought on that occasion the virus was brought to the US in infected prairie dogs. They had been kept as pets and housed with Gambian pouched rats and dormice that were imported from Ghana. Other cases – usually in people who had recently travelled to African countries – have been seen in the UK, Israel and Singapore.
But since May 2022 there have been a spate of outbreaks reported in the US, UK, Australia, mainland Europe, and Canada. While this has worried health authorities and scientists, the number of infections in these outbreaks are a fraction of those seen in Africa, where the disease is endemic. A major outbreak in the Democratic Republic of Congo has seen more than 19,000 cases and 900 deaths since January 2023. The version of the virus causing the DRC outbreak is a more deadly version, known as clade I, compared to the version that caused the 2022 outbreak in the US, known as clade II.
The US Centers for Disease Control and Prevention says the risk posed to the US by the type of mpox circulating in the DRC is low and that people who have been fully vaccinated, or have had mpox previously, should be protected against the clade I virus. No cases of clade I virus have yet been reported in the US.
Exactly where the surge in outbreaks since 2022 originated, however, is still something of a medical detective story. Genetic analysis has revealed that the variant of the virus causing the outbreaks belongs to a branch of the mpox evolutionary tree that initially appeared in West Africa, but no clear link to any countries where the virus is endemic has been found. Instead, there is now the suspicion among health experts that the virus might have been circulating undetected in human populations in a number of countries outside Africa for several months, if not longer.
Some genetic analysis – although still preliminary and yet to be peer-reviewed – has indicated that the West African mpox virus (clade II) may have picked up the ability to spread from human to human as early as it could have been as early as 2017. And since then it has accumulated a high number of mutations that have made it better able to infect and pass between human hosts – including one that may help it to inhibit some of our immune defences.
More recently a new variant of the mpox virus, known as clade Ib, has appeared in the DRC and appears to spread more easily through close contact. It seems to have first emerged in the area around the city of Goma, north Kivu, and is particularly prevalent among children under the age of 15 years old. Research suggests the variant could have begun circulating as early as September 2023.
How does mpox spread?
Unlike the virus that causes Covid-19, which primarily spreads through tiny droplets expelled as we breathe and is highly infectious, mpox is not as readily transmissible. It instead relies on close physical contact – usually prolonged – to pass from person to person, or animal to person.
"It could be contact with someone who has an infectious rash, such as lesions, scabs and bodily fluids," says Madeline Barron, from the American Society for Microbiology (ASM). "You can also get it by touching items that someone who's infected may have touched."
A study published in the New England Journal of Medicine found that between April and June 2022, 98% of the infections in 16 countries were in men who have sex with men, but it's not clear why this is the case. It could just be coincidence – once a disease is introduced to a community, it tends to spread within that community. And there is no evidence that mpox passes any quicker through a population of men who have sex with men than any other group. Nor is there any evidence that it is more infectious to men than women.
"We don't know if the virus can spread specifically through sexual transmission routes, such as through vaginal secretions or semen, but it seems to be that intimate contact is promoting the spread," says Barron.
Although DNA from the mpox virus has been detected in semen by researchers, it does not necessarily mean that this is how it is spreading. The mpox virus is a packet of genetic information encased in an envelope of proteins and a membrane. It requires all these components to be in working order if it is to infect cells, and although viral DNA can be detected in semen, the virus itself may not be viable and capable of infection.
How dangerous is mpox?
Another important thing you need to know about mpox is that it is deeply unpleasant. Compared to the Central African strain of the mpox virus, the West African version is generally associated with milder disease and fewer deaths. The mortality rate of the clade I strain is about 10%. For those infected by clade II, 99.9% survive. As of June 2024 there had been 99,176 confirmed cases since the outbreak began in 2022 according to the WHO and 208 reported deaths.
But even if the chances of dying are relatively low, patients with monkeypox have reported how painful and debilitating it is.
"It's long, it's nasty and you don't want to get it," says Barron. "People may feel flu-like symptoms in the beginning, with fever, headache, stuff like that, but as the disease progresses you get a multi-stage rash, lesions can develop in your mouth, your feet and genital region and these develop into pus-filled blisters."
 Getty Images
Getty ImagesIt can take between five and 21 days from infection before symptoms start, although typically this incubation period is 6-13 days. Initially it begins with headaches, fever, muscle aches and fatigue for the first few days. One distinguishing feature of the virus is swelling of the lymph nodes. Eruptions on the skin tend to appear within a couple of days of the fever appearing.
Some three to four weeks after infection, the blisters will eventually scab over and fall off. Scarring, however, is common in people who recover. There is no specific treatment, other than medicines to treat the symptoms, and, like most diseases, your chances of getting seriously ill or dying depend on factors such as your age and level of immunity.
What perhaps makes monkeypox so shocking is that the symptoms look similar to a disease of the past. One that we thought we had seen the back of thanks to a successful global vaccination campaign: smallpox. Monkeypox is from the same group of viruses as smallpox, although a distinct virus. (Read more about the mysterious virus that helped us eradicate smallpox.)
Is mpox evolving?
Mpox is a brick-shaped virus carrying a double-strand of DNA. This is good news because it means the virus is relatively stable and less likely to mutate into more lethal or more transmissible variants. The Sars-CoV-2 virus that causes Covid-19 contains genetic material made from a single stranded RNA.
"RNA viruses mutate very effectively – they're diabolical, in my opinion, they're just really nasty viruses," says Rodney Rohde, a professor at Texas State University with a background in public health and virology. He is the co-author, with Barron, of a 2022 publication for the American Society of Microbiology on the current state of knowledge about mpox. "DNA viruses typically don't mutate that quickly, even with the 50 mutations we've seen (in mpox), so we don't see mutations having an impact on the severity of the disease."
 Melina Mara/The Washington Post/Getty Images
Melina Mara/The Washington Post/Getty ImagesPart of the reason for this may be because more than half of the mutations seen in the virus between 2018 and 2022 are considered to be "silent" – meaning they don't change any of the viral proteins it needs to infect cells and evade the immune system. Even so, some researchers have expressed surprise at how many mutations the virus has accumulated in the three or four years leading up to the 2022 outbreak. Researchers identified two distinct lineages of the virus – suggesting separate sources – spreading in the US. there is some evidence that the virus may have been circulating silently and undetected for around 20 years outside Africa.
The new cluster of patients with the clade Ib mpox variant in the DRC suggests the virus has been evolving rapidly. It showed a high mutation rate, including some changes in its genetic code that could have helped the virus spread more easily from human to human.
Preliminary unpublished research has also identified potential mutations that have yet to be seen in the virus but could alter how pathogenic the disease becomes if they were to occur in the future. But this work, if shown to be correct, could also help health officials and scientists look out for signs mpox is evolving into something more worrisome.
Why mpox became a global health emergency?
The WHO briefly declared mpox to be a public health emergency of international concern in July 2022 but it was then declared over by May 2023 due to progress in tackling the disease. However, the risk posed by mpox has grown, and in August 2024, the Africa CDC declared a public health emergency on the continent due to the rapid spread of new variants of the virus. On 14 August 2024, the WHO declared the surge in mpox cases in Africa a public health emergency of international concern. It rasied particular concern about the number of cases in the DRC, where the 15,600 cases and 537 deaths have already exceeded the number for the entire year of 2023.
Among the reasons for the concern lie in mpox's relationship to smallpox.
For almost 200 years, we had been routinely vaccinating people against smallpox. Today, thanks to a global scientific effort, smallpox is the only human disease we have wiped off the face of the Earth, and the world was declared smallpox-free on 8 May 1980. Although the smallpox virus still exists in secure laboratories, it is no longer a transmissible disease. But neither do we now have any natural immunity to smallpox or similar viruses. And with the end of the smallpox vaccination campaign in the mid-1980s, so too has the protection it offered against other pox viruses waned.
"We probably had a pretty strong herd immunity across the globe when we eradicated smallpox," says Rohde. "There's some research that shows that if you go back and look at the population in Nigeria, for example, they probably would have spread monkeypox more efficiently had they not been vaccinated against smallpox.
"Once we stopped smallpox vaccinations, we had waning antibodies – my parents, for example, may have some immunity, but it's probably really poor."
How effective are the vaccines?
The good news is that vaccines developed for smallpox are effective against mpox – up to 80% effective. And, even though there have been recent moves to destroy stockpiles of smallpox vaccines around the world, countries have been replenishing their supplies. Mostly, however, this has occurred in wealthy nations. And that's perhaps the most dispiriting aspect of this most recent monkeypox outbreak. We have known about the disease for more than 50 years but only when it spread to North America and Europe did governments outside Africa appear to take any notice.
Data from the Africa Centres for Disease Control and Prevention shows that, since the beginning of 2022, there have been some 1,267 confirmed mpox cases across the continent, with at least 285 deaths.
 Mike Roemer/Getty Images
Mike Roemer/Getty Images"Many of us have been screaming about these types of issues for decades," says Rohde. "In my opinion we don't always think about these things when they're not on our shores."
"Those regions where it is endemic, and it's been a prolonged issue, are still at the short end of the stick in terms of getting the resources, the diagnostics, the vaccines, everything needed to handle the outbreak," adds Barron. "If Covid has taught us anything it's that the world is small and you need a coordinated effort to respond to diseases because diseases don't know boundaries."
A 2020 United Nations report warned of the growing risk of new diseases passing from animals to humans, exacerbated by our encroachment on natural habitats and the effects of climate change. The bottom line for Friant, who specialises in the health consequences of the interaction between humans and animals, is that we need better monitoring of all potential zoonotic diseases.
"We need more investment in understanding the diseases and preventing that initial spill-over event from animals to humans from happening," she says. "We also need collaboration and capacity building in countries so that they're equipped to respond to these events – it definitely shouldn't just be about protecting the Western world."
Like Covid-19, mpox is just the latest disease to spread from animals into the human population. Given its relatively slow spread and the fact that vaccines are available to prevent infection, it's likely mpox outbreaks can be contained. But monkeypox won't be the last disease of this nature. And the world will need to be ready and vigilant for the next.
* This article was originally published on 2 August 2022. It was updated on 20 May 2024 and again on 13 August 2024 to include details of outbreaks in DRC and some of the latest research on the virus evolution.
--
If you liked this story, sign up for The Essential List newsletter – a handpicked selection of features, videos and can't-miss news, delivered to your inbox twice a week.
