The global fight against snake bites

 Sushil Chikane/Alamy
Sushil Chikane/AlamyVenomous snake bites are responsible for 138,000 deaths every year around the world, but could some disarmingly simple interventions help to save lives?
"In the monsoon, the fields are overgrown with weeds," says Tukaram Rao, a farm labourer from the village of Rathnapuri in Karnataka, south-west India. "We have to walk out in the midst of those at night to turn on the water pump for the field. Sometimes if the water pipes are disjointed, we walk alongside the water pipe, feeling with our hands to fix it."
Like many farm workers in rural India, Rao and his neighbours tend to get around barefoot. But lurking in the thick undergrowth is something more worrisome than leaking water pipes. This is the perfect habitat for the Russell's viper, a large, earth-coloured and highly venomous snake found across much of India and other parts of South Asia.
These snakes are mainly active during the night and are masterful ambush predators, remaining motionless for long periods before striking ferociously at their prey. They mainly hunt rodents or small frogs that scurry into their path in the fields where they forage – these snakes are not interested in humans. Yet they account for more bites and deaths in India than any other species of snake. The Russell's viper is estimated to be responsible for as many as 43% of snake bites in India and is responsible for 30-40% of snake bites in Sri Lanka.
Much of the reason for this is how they hunt. Sluggish to the point of immobility, they inch their way through the grass, their green and brown camouflage making them almost invisible in daylight. At night, they are impossible to spot. For farmers working in paddy fields or among overgrown plants, the snakes are easy to step on or disturb. And when they feel threatened, the Russell's viper quickly becomes aggressive, striking out at random with its fangs.
 Alamy
Alamy"Sometimes they go away, sometimes we end up getting bit," says 48-year-old Rao about the snakes they encounter when working in the fields. Most villagers are scared of the snakes, he says and usually run away when they come across one in the field.
This fear is perhaps well founded. There are around 2.8 million cases of snake bites in India each year and 50,000 deaths. In the past two decades, more than 1.2 million people have died from snake bites in India alone, according to one recent analysis. Globally snake bites are thought to cause between 81,000 and 138,000 deaths each year, according to some estimates.
But the true impact of snake bites is greater still. A bite from a venomous snake can leave survivors with life-changing injuries. It is something Rao has seen first-hand.
"Another farmer was recently weeding his turmeric field when he accidentally got bit on his leg and the flesh around his ankle rotted away," he says. "The rot spread to his knee. Now he is unable to do any work." Doctors were eventually forced to amputate part of the unfortunate man's leg and his wife has had to take on extra work to provide for the family, Rao adds. It is not an uncommon story.
"Three times as many victims – around 400,000 per year – are left with long-term disabilities such as limb necrosis leading to amputations, disfigurement and blindness," says Laura-Oana Albulescu, who studies snake venom at the Liverpool School of Tropical Medicine in the UK. "The psychological sequelae are only now being investigated but are significant as people can end up unable to work, destitute from the treatment cost, not fitting into their society – disabled young girls are not able to work or marry."
The global health burden created by snake bites is thought to be huge. Of the estimated 4.5 million people who are bitten by snakes worldwide each year, around 2.7 million men, women and children are left seriously injured, according to the Global Snakebite Initiative, a non-profit organisation aimed at addressing the problem of snake bites.
"Snake bites are a far bigger problem than many people realise," explains Leslie Boyer, founding director of the Venom Immunochemistry, Pharmacology and Emergency Response (Viper) Institute at the University of Arizona in the US. The World Health Organization considers snake bites to be such a burden on some communities that they recently classified snake bite envenomation – where venom is injected by a bite – as a neglected tropical disease.
You might also be interested in:
Snake bites are now recognised as one of the world's most important neglected health problems and one that disproportionately affects poorer communities.
But should snake bites be such a large problem? "We've known how to make antivenoms for about 120 years," says Boyer, referring to some of the early work by scientists at the Pasteur Institute in France, the Lister Institute in England and the Butantan Institute in Brazil. While many antivenoms are relatively effective, the complex nature of snake venom can make treatment difficult. Access to antivenom can be patchy and treatments with it can be expensive.
This has led some to seek other ways of tackling the health burden caused by snake bites.
Rao and his neighbours are now involved in one such project aimed at helping the communities most at risk from snake bites to protect themselves. And the solution is deceptively simple – they are being given boots.
 Sumanth Bindumadhav/HSI
Sumanth Bindumadhav/HSI"Many people in rural parts of India are walking around in the dark without footwear," says Sumanth Bindumadhav, senior manager of the wildlife, disaster response and Dharwad program at the Humane Society International in India. "Over 90% of bites occur when people step on a snake without even seeing them."
His organisation has handed out more than 400 rubber boots and 200 solar lamps to residents in Rao's village and the surrounding area. "Putting a light in people's hands and footwear that will cover up to the ankle can seem simple, but it makes a big difference," says Bindumadhav. "The Russell's viper has some of the longest fangs of any snake in India, but it is very hard for them to penetrate gumboots. And preventing snake bites is better than treating them."
Snake venom is a complex cocktail of toxins that varies from species to species. Some of the enzymes and small proteins found in snake venom interfere with the signals sent by nerve cells. Depending on the exact toxin, these can lead to rapid, painful muscle contractions or paralysis. Victims often suffocate as the muscles controlling the respiratory system malfunction.
Other toxins, such as those found in black mamba venom, bind to heart muscle cells to prevent them from beating. Some toxins often found in viper venom cause victims to bleed to death by preventing blood clotting while others can cause blood cells to break down, starving victims of oxygen. There are toxins that cause the blood to coagulate in a bite victim's veins or attack the cells of key organs in the body. There are also venom toxins that trigger extreme inflammation or lead to necrosis, where the tissue on a limb dies and rots away.
Many snakes have a combination of different toxins that can cause a number of these effects at once. It means treating snake bites is no simple task.
"Any one snake bite contains hundreds of toxins in different proportions that vary by individual species," says Boyer. "You can't use a single small molecule drug against something like that."
Fortunately, antivenom is relatively easy to make, provided you have the know-how and access to some horses. At its most basic, antivenom is made by collecting venom from the snake you are interested in (a process known as "milking"), injecting a small amount into a horse and then collecting the antibodies it then produces. These are then purified and can be injected into bite victims to neutralise any venom toxins they encounter.
But it is not always effective and can require large amounts of antivenom as the number of antibodies in each dose can be low.
"Depending on the snake bite, it can take between one and 20 vials of antivenom, and there are cases in the US that have gone to 100 vials," says Boyer. In one study in South Africa, for example, snake bite victims received an average of five vials of antivenom each, but at some hospitals that figure was 19 vials per patient.
The low levels of antibodies that target venom toxins in antivenom can also lead to other problems such as anaphylactic shock as the patient's immune system reacts to the animal antibodies in the antidote – a condition known as serum sickness. "Unfortunately, only 15-20% of the antibodies are specific to and will neutralise venom toxins, hence the adverse reactions," says Albulescu.
Antivenom can also be very expensive. Depending where you are in the world, a single vial can cost anything from $18-200 (£13-£145) in Sub-Saharan Africa to $17,000 (£12,362) in parts of the US. Boyer's own research group was instrumental in developing a rattlesnake antivenom sold in both Mexico and the US. It costs around $100-200 per vial (£73-£145) in Mexico but can cost several thousand dollars in the US. When she analysed the difference in costs between the two countries, Boyer found that much of the difference in price is due to the way healthcare is funded rather than production costs. "Developing and manufacturing antivenom is a very small piece of the pie," she says.
In Latin America, where venomous snakes are also a major problem, there has been a long history of domestic antivenom production from countries such as Mexico, Brazil and Argentina that has helped to keep prices low and a steady supply, says Boyer. But legal, regulatory and hospital costs, alongside the idiosyncrasies of the US medical insurance system have driven up prices 1,000-fold in the US. Relatively low demand for venom in the US and Europe – around 7,000-8,000 people are bitten by snakes in the US annually – also leads to higher prices.
This has knock-on effects for other parts of the world that have to rely on imported antivenom, Boyer adds. "It is difficult to rear horses in areas where there is African horse sickness, so many countries in Sub-Saharan Africa are reliant upon importing antivenom from Europe," she says. "Even though antivenom is cheaper there, it can still cost many times the annual wage of a worker."
 Minden Pictuers/Alamy
Minden Pictuers/AlamyIndia has some of the cheapest antivenom in the world, costing around $6.5-11 (£4.7-8) per vial, but problems with quality and availability often mean patients do not get the treatment they need.
"Every year there is a shortage of antivenom," says Bindumadhav. Rural communities particularly struggle to get treatment and are disproportionately hit by the consequences of snake bites due to the wider costs of treatment and loss of income that can result.
"It tends to be the lowest strata of society who are getting bitten in the countries with the highest number of snake bites," says Bindumadhav. "It is farmers and labourers rather than politicians and business leaders who are being bitten." This means the problem is largely overlooked.
Hospitals in India also primarily use a polyvalent (or multipurpose) antivenom as an antidote against the "big four" snakes that cause the majority of bites – the spectacled cobra, the common krait, saw-scaled viper and the Russell's viper. It is produced using venom from these four snakes. But India has more than 60 venomous species of snake and there is no specific antivenom against most of them. Instead, the "big four" antivenom is often used as a general snake bite treatment. Recent research has found, however, that it is largely ineffective against the venom of other important snakes in the country.
To compound the problem further, other research has shown that even among the big four, the toxins in the venom can vary depending on where in the country they are. It means that antivenom produced using snakes in southern India might be less effective against the venom from the same species in the north or those in Sri Lanka or Nepal.
Recently the Wellcome Trust launched a major new initiative to develop new drug treatments for snake bites in an effort to address the shortcomings of current antivenom treatments. It estimates that just £57m ($79m) was invested into research on snake bites in the decade between 2008-2017. It has pledged to spend £80m ($110m) over seven years on new research.
Some researchers are focused on new antibody-based treatments that work against a wider range of snake venoms or induce less side effects. One approach has been to use camels instead of horses to make antivenom while others are attempting to manufacture human antibodies against snake venom, but both approaches are too expensive to yet be used commercially.
Instead, some researchers are turning to other types of drug treatments that can work against some of the nastier components of snake venom.
Albulescu is among them. She has found that a drug used to treat heavy metal poisoning in Germany called DMPS could be repurposed to be used as a first line intervention against the venom of saw-scaled vipers. This family of snakes, also known as carpet vipers, are found across Africa, the Middle East, India, Sri Lanka and Pakistan. When threatened they rub the scales on their body together to produce a distinctive sizzling sound, and they possess a highly toxic venom that contains enzymes known as metalloproteinases. These rely upon a zinc molecule in their structure to degrade the cell membranes of blood vessels and break down the structures there, leading to haemorrhaging that causes victims to bleed to death.
 Ezequiel Becerra/AFP/Getty Images
Ezequiel Becerra/AFP/Getty ImagesAlbulescu found that DMPS can capture the zinc in the metalloproteases and stop them from functioning. "It's formulated as an oral capsule and can be administered easily in the field immediately after a bite," she says. "We propose its use as a first line intervention which can neutralise some of the venom toxicity and prevent the onset of systemic haemorrhage, buying the victim time." When DMPS was combined with a later antivenom treatment, Albulescu and her colleagues found survival in animal models increased to 100%.
Of course, transferring such a treatment into humans and into the imperfect world of real-life situations, where giving such drugs in a timely fashion might be difficult. And saw-scaled viper venoms contain other unpleasant toxins that DMPS does not act against.
Drugs that work against a wider range of snakes are also more desirable as often snake bite victims do not know exactly which species they have been bitten by. If the snake is misidentified, it can lead to inappropriate treatment.
Albulescu and her team have made some progress, finding a mixture of two other toxin inhibitors that appear to work against a wider range of viper venoms including the Terciopelo, or fer-de-lance, in Central America, the puff adder in Africa and the Indian saw-scaled viper. Another group at the University of Copenhagen in Denmark recently announced that they had developed a drug that works against the neurotoxins found in many snake venoms, including those of cobra.
The hope is eventually these could lead to drugs that can be easily stored and carried in first-aid kits as a way of reducing the potency of snake venom to buy victims some time.
"These are never going to be one-size-fits-all treatments," says Boyer. "But they could be a bridge to antivenom. It could help someone survive the trip to a hospital where they stock antivenom or protect a limb from necrotising damage. It might also reduce the amount of antivenom that is needed."
 Sumanth Bindumadhav/HSI
Sumanth Bindumadhav/HSIBut she adds that many of these small molecule drug treatments have yet to be proved in clinical settings. And they too could suffer from the same economic pitfalls as antivenom unless efforts are taken to keep prices low. Instead, Boyer is more excited about innovations that are taking place outside of the laboratory to keep people safe from snake bites.
"These are more about sharing knowledge so people can take care of their own and educating people about snakes," she says.
One such example is the Asclepius Snakebite Foundation, an international group of researchers and medical professionals who train local doctors and nurses in Africa to manage snake bites alongside public health initiatives to help protect people from being bitten. They help local people understand where the risk of encountering snakes is high and how they can reduce them, such as moving debris away from houses. They also train motorcycle taxi drivers in basic snakebite first aid so they can transport patients from remote locations to treatment centres.
In India, the Humane Society International has also been working to train doctors in the region around Karnataka to deal with snake bites, but it is also trying to educate rural communities with simple ways to reduce their risk too.
The Indian krait, for example, is one of the "big four" snakes responsible for the majority of venomous bites in India. The venom of the common Indian krait can kill within a few hours and a higher proportion of its victims appear to die compared with other snakes. But it can be thwarted by a few simple steps, says Bindumadhav.
"It has a dubious reputation for biting people while they are asleep on the floor," he says. "A simple solution is to have a mosquito net hung from above and tucked under the mattress. In India a net like this costs a dollar. It is not expensive."
But Bindumadhav says there are other challenges. "There is still a tendency for some bite victims to be taken to a faith healer rather than to hospital," says Bindumadhav. "The Russell's viper doesn't always inject venom when it bites – these are dry bites but the panic they cause can lead to psychological symptoms instead. Then they appear to get better after a trip to the healer. Unfortunately, in those cases where venom is injected, it means their treatment is delayed."
Knowing whether a bite victim has been envenomed is a challenge, particularly when antivenom treatments are in short supply. Some researchers are working on techniques to help them identify whether a bite victim has been injected with venom by using thermal imaging cameras.
"Most snake venoms, and for that matter many other animal venoms, result in tissue inflammation at the site of a bite," says Tamilarasu Kadhiravan, a professor of medicine at the Jawaharlal Institute of Postgraduate Medical Education and Research in Puducherry, India. "Venom-induced inflammation is accompanied by an increase in skin temperature, which is seen as hotspots on infrared images."
He has found that the tissue around envenomated bites tends to be between 1-3C higher than the surrounding skin. He and his colleagues have used the technique to help identify which snakebite patients might need most attention.
"We treat 200-250 patients with snake bites every year," Kadhiravan says. "Antivenoms are a precious resource. Typically, in our setting, treatment with 20 vials of antivenom for a single patient costs about $70 (5,278 Indian Rupees/£51)." He says using an infrared imaging camera costs around $1 (75 Indian Rupees/£0.73) per patient. "If infrared imaging could prevent wasteful use of antivenom in situations where it is not really indicated, it could be used to treat more patients who actually need it."
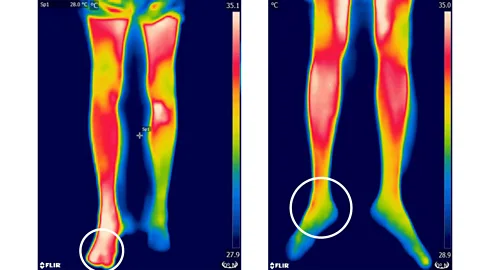 P. Sabitha et al/Plos Neglected Tropical Diseases
P. Sabitha et al/Plos Neglected Tropical DiseasesTechnology is also helping with identification of snake species themselves, which in turn can also help to make treatment more effective.
Doctors in Nepal and Switzerland, for example, have been developing genetic testing techniques to help identify the snake species responsible by analysing swabs taken from bite marks. While they found they could identify some of the species responsible, it only worked in around a quarter of cases and the technique still takes too long to be used effectively in an emergency setting to identify snakes.
Instead, artificial intelligence could also offer some assistance by helping to identify snake species from photographs taken by eyewitnesses to a snake bite. Many victims of bystanders take images on their mobile phones to assist in identification, but unless a medical professional is trained to tell the difference between species, these can be of little use. Isabelle Bolon, a vet at the University of Geneva, in Switzerland, and her collaborators are developing an app that uses machine vision algorithms to automatically identify snake species. Knowing which species is responsible could not only ensure patients get the right treatment more quickly, but also help to build up a more accurate picture of which snakes are really responsible for bites.
In Rathnapuri, India, the Humane Society International in India have been working alongside the conservation initiative The Liana Trust to understand more about the snakes that live around the villages by learning about their behaviour. Working with locals, Bindumadhav and the team have attached radio tags to around 30 snakes, allowing them to track and record the snakes' behaviour over a three-year period.
 Jeff Rotman/Alamy
Jeff Rotman/Alamy"Every morning we find the snakes, look at what habitat they are in, whether they are shedding their skin or have just fed," he says. "We are looking at how close they are to where people are working, where they are moving. It is giving us a lot more accurate information that we need to help tell people how to avoid and respect the snakes."
Involving local people in this research has also been crucial as it is helping to overcome local resistance to the interventions they are attempting to introduce, says Bindumadhav. Farmers, for example, often prefer not to use boots or flashlights when working in the field as they impede their ability to move around or to do work quickly. Similar schemes to hand out boots in Africa have failed because villagers found the boots uncomfortable and as the rubber was valuable, they sold them off, says Albulescu. Boyer too has heard of similar problems.
For farmers like Tukaram Rao, knowing more about the snakes has helped to dispel much of the fear that surrounds them.
"Before this, we used to be very scared of snakes," he says. "We used to run away on seeing a snake or not work in that area at all. Now we have some basic knowledge. For example, when we go to work, we use a stick to check the area before we start working."
Rao had his own close encounter with a Russell's viper recently while walking from his house to secure his cows. "I first noticed something shining in the pathway," he says. "I asked my son to fetch a light and we drove it away."
He hopes that as they learn more about Russell's vipers and their behaviour, it could ultimately allow his community to live alongside the snakes rather than in conflict with them.
"Many people used to kill snakes on sight," he says. "But as we understand them better it could lead to fewer snakes being killed."
Bindumadhav's ambitions are greater still. He wants to make the entire district around the village free from snake bite deaths. "We are starting with a village," he says. "But we hope to scale it out to other districts. Snakes are misunderstood creatures – there is no reason anyone has to die from them."
* This article has been updated on 15 April 2021 to reflect an change in the estimate for spending on venom research. Recent research commissioned by the Wellcome Trust found £57m had been spent between 2008-2017 rather than its earlier estimate of £30m.
--
If you liked this story, sign up for the weekly bbc.com features newsletter, called "The Essential List". A handpicked selection of stories from BBC Future, Culture, Worklife, and Travel, delivered to your inbox every Friday.
