The 'unwarranted hype' of stem cell therapies
 Alamy
AlamyClinics claim that expensive stem cell therapies can help patients with dementia, autism, multiple sclerosis and even cerebral palsy - and crowdfunding campaigns to pay for the treatments are increasingly common. But are the patients and the donors being misled about the benefits and the risks?
Jay Shetty is 8 years old. He is smart and bright, says his mother Shilpa, even if he can’t do all the things his younger brother can. “Jay doesn’t sit up or use his hands much. He’s non-verbal and we don’t know how well he can see,” she says. “But he plays with us and tries to copy everything his younger brother Kairav does.”
Jay has cerebral palsy. In his early years, Shilpa was desperate to find anything that might help him. Scouring the internet late each night, she read about a stem cell trial at Duke University in North Carolina but Jay wasn’t eligible. When Kairav was born in 2015, Shilpa and her husband stored their younger son’s umbilical cord blood, which was rich in blood stem cells, hoping another trial would emerge. It did, and this time, children with sibling cord blood could participate. Was she worried about the risks for Jay? “It wasn’t invasive and it couldn’t do any harm really.” To raise the £15,000 ($18,200) treatment bill, they supplemented money they had already fundraised for private physiotherapy and hydrotherapy with a personal loan and a further fundraising push supported by the cord bank where Kairav’s cord blood had been stored.
Cerebral palsy is a group of lifelong conditions that affect movement and coordination. In Jay’s case, Shilpa explains, there were complications around the time of his birth that led to the condition. There is no cure for cerebral palsy but physiotherapy, speech therapy and occupational therapy can help some symptoms. Shilpa hoped, though, that Jay’s stem cell therapy – a two-hour infusion into his veins – would bring benefits far beyond everything they had tried before.
 Getty Images
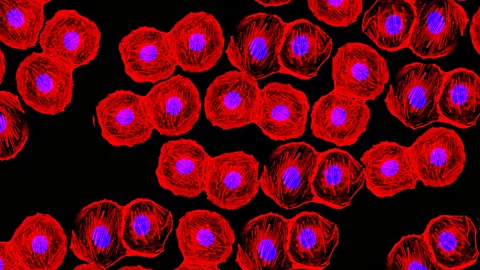
Getty ImagesWe all have stem cells – these are building-block cells of sorts, with the ability to develop into a wide range of specialised cell types, such as muscle, skin, or brain cells. Stem cells not only replenish our old cells but also spring into action to repair and replace injured tissue. As a result, they have been likened to our own army of microscopic doctors, but that army is relatively small.
The excitement around stem cell therapy revolves around the ability to grow more of these cells in the laboratory so they can be used to produce new tissue, replace damaged cells, and unravel disease mechanisms.
You might also enjoy:
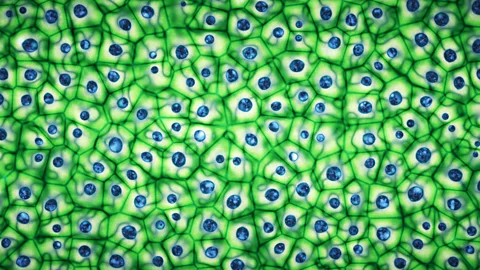
So far, researchers have primarily focused on developing two different types of stem cells: embryonic and adult. Embryonic stem cells, which are extracted from a growing embryo, have the natural advantage of being able to give rise to any other cell in the body, an attribute known as pluripotency. But some people have raised ethical concerns about the use of embryos in deriving these stem cells – issues that are circumvented by the use of stems cells harvested from adult tissues. Adult stem cells are not naturally pluripotent, which means they tend to be more specialised and so only able to develop into a narrower range of cell types. They can be re-programmed, however, to regain that developmental flexibility.
Stem cell therapies certainly do hold genuine promise for certain disorders. Proven and licensed stem cell-based treatments already exist for blood and immune conditions such as leukaemia, lymphoma and myeloma. It is also approved in some countries for chemical burns to the eye.
Hopes of using stem cells to treat other disorders have inspired many new clinical trials and driven a “stem cell tourism”, centred in Ukraine, Panama and Thailand. By 2018, there were over 432 US-based business at 716 clinics engaged in direct-to-consumer marketing of stem cell treatment.
These clinics universally share one feature: eye-watering fees – and even trials like the one at Duke University have a hefty price tag.
 Getty Images
Getty ImagesThat’s where crowdfunding comes into its own. A recent study in the Journal of the American Medical Association identified 408 US campaigns for stem cell treatment on YouCaring and GoFundMe, with more than $7m sought and 13,050 donor pledges. The clinics often actively encourage these campaigns: one at Northwestern Medicine has a handbook with a section on “soliciting methods”.
The campaigns often underplay potential risks or omit them entirely:
“It’s that simple and quick, and with only minimal side effects,” claims one page attempting to raise funds for a man with Parkinson’s.
“Most importantly it has been shown to slow the disease progression without any side effects,” describes another, raising funds for someone with amyotrophic lateral sclerosis (ALS) – a common form of motor neurone disease.
Only 26 of those 408 campaigns mentioned ‘risk’ and even then as risk-free or low-risk compared with alternative treatments.
It’s understandable that campaigners might underplay the dangers – donors might not contribute otherwise. But these cases tell another story:
- In 2017, Doris Tyler, a 77-year old former music teacher raised money on GoFundMe to cover stem cell treatment in Georgia (US) to treat age-related macular degeneration (ARMD). “We love you, Doris!” one supporter wrote. Before treatment, she was able to read large-print books and navigate her home. Tyler is now almost blind: “When I wake up in the morning one of the hardest things is opening my eyes and seeing that everything is still dark. And it’s going to be this way until I go to sleep.” At least three other patients with ARMD lost their vision following stem cell treatments in Florida in 2015.
- At least 17 patients were hospitalised over the past year in the US after umbilical cord blood injections. The Centers for Disease Control confirmed a series of bacterial infections. Most of these patients were treated at orthopaedic, chiropractor and pain clinics and were given injections into their spines, knees, and shoulders.
- Following a stroke in his early 60’s, Jim Glass sought stem cell treatment in Argentina, China, and Mexico (cost: $200,000). A spinal cord tumour subsequently paralysed his right leg (the stroke had already paralysed his left). DNA analysis indicated the tumour arose from the injected stem cells.
- A nine-year old boy developed multiple brain and spinal cord tumours following stem cell transplant. Pathological analysis confirmed the spinal tumour contained cells from at least two donors.
Where crowdfunding campaigns fail to reference risk, it could be because some clinics themselves barely convey it. Paul Knoepfler, a biomedical scientist at the University of California, Davis School of Medicine, turned up to one clinic’s self-styled educational seminar (used to recruit patients, promising large discounts upon sign-up). Staff, mostly dressed in medical scrubs, neglected to mention any potential adverse events associated with stem cell transplants. The audience did, however, receive a credit application form to complete. Knoepfler wrote that the experience was “more like attending a persuasive entertainment show or something on a television shopping network than an educational seminar”.
 Getty Images
Getty ImagesAs well as underplaying the risks of these therapies, crowdfunding campaigns sometimes overstate its benefits.
“Stem cell treatment has helped thousands of children with autism,” said one. This campaign, aiming to send a young boy to Panama has raised over $18,000 since September, surpassing its $15,000 goal.
“The ALS patients all said it reversed the damage that ALS did to them! Breathing gets better, speaking and swallowing gets better people in wheel chairs were walking in two weeks,” claimed another. This campaign raised $1,040 of this patient’s $300,000 target to date.
Yet many experts argue that these claims are premature.
There is currently no proof that stem cell treatment is effective for autism, as Alycia Halladay, chief science officer at the Autism Science Foundation, wrote in Scientific American last year. Arnold Kriegstein, professor of neurology at the University of California, San Francisco, has similarly emphasised that recent autism trials using stem cell transplant have failed to confirm its efficacy, despite claims to the contrary. He describes the research as “premature”.
Using stem cell treatments in ALS is especially challenging. Even if transplanted cells are able to migrate to the areas of damage, mature and integrate into a patient’s nervous system before the disease takes its toll (life expectancy is variable but averages two to five years from the time of diagnosis), they will encounter a hostile environment with motor neurons dying around them. At present, most trials are instead focused on using stem cells to create laboratory models of motor neurones on which drugs can be tested and disease mechanisms studied. The MND Association believes that stem cell research is essential in understanding, preventing and curing MND but state: “at present, there is no reliable evidence to suggest that stem cells can be used as an effective treatment”.
That Journal of the American Medical Association study found 43.6% of campaigns carried statements that were definitive or certain about the effectiveness of treatment. It’s not too difficult to trace these overstated claims back to some clinics that use “tokens of scientific legitimacy” – published articles in journals with little or no peer-review in addition to implied links to preclinical research at reputable but unaffiliated research centres.
 Alamy
AlamySometimes the media has helped spread the unfounded hype. In 2014, former soldier James DeLittle, diagnosed with Parkinson’s, paid £7,000 ($8,500) for a stem cell procedure in Ukraine. Afterwards, the press frequently quoted the clinic’s claim for improvement in 75% of their patients. “After just one of the two treatments, the doctor asked me to touch my nose with my eyes closed and I was spot on — I couldn’t believe it,” said DeLittle at the time. “My Parkinson’s feels like there is a spring which constantly pulls me to the left hand side. But immediately after the treatment the force didn’t feel as strong and my balance was much better as a result.”
Two years later, a deteriorating DeLittle told the BBC he felt “annoyed, out of pocket and, conned”. Yet most of those 2014 readers will never know that the man who hoped that a stem cell treatment would be “a miracle in the making” eventually concluded it was nothing more than a scam.
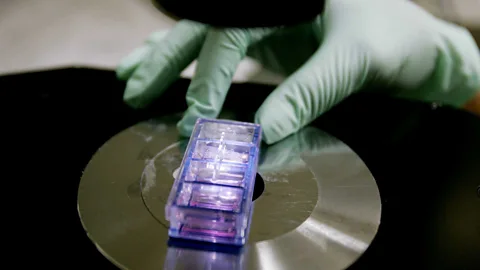
Patients might not even get what they’ve paid for (let alone foregoing effective treatments). Lisa Fortier, regenerative medicine researcher at Cornell University, tested nine products but “none contained stem cells, or a single live cell of any kind”. So, people are potentially crowdfunding for, and donors contributing to, putative stem cell treatments that have no stem cells.
Not all stem cells are created equal, either. Some trials use mesenchymal stem cells – these are cells found in bone marrow, for instance, that are important in making and repairing skeletal tissues, such as cartilage, bone and fat cells. But these are now serious questions about whether they even function as stem cells. Even the person who first named them, Arnold Caplan, believes they should be renamed to quell unadulterated hype about their potential: “I was wrong. I take back the name that I gave these hugely important cells.”
 Getty Images
Getty ImagesNone of which is to deny the potential for future (authentic) stem cell therapies to help some neurological conditions. The neurodegeneration in Parkinson’s is relatively focal – dopaminergic neurons are progressively lost in a specific region called the midbrain – which makes it a good potential candidate for cell replacement for some of its symptoms. A Kyoto University trial is using induced pluripotent stem cells, developed by reprogramming skin and other cells to revert to an embryonic-like state. These become ready to morph into other cell types, in this case, dopamine precursor cells. “We made a hole in the frontal part of the head's left side and transplanted some 2.4 million cells,” researchers excitedly said of their first patient, at the beginning of their two-year trial. Parkinson’s UK remain optimistic about the potential of stem cell transplants but emphasise research must continue within the UK’s “rigorous ethical and regulatory framework”.
A more prominent surge in interest has centred around multiple sclerosis. Autologous haematopoietic stem cell transplantation (AHSCT) aims to replace or reboot the body’s immune system: high doses of chemotherapy wipe out a patient’s existing immune system which is then rebuilt using their own stem cells collected before chemotherapy.
AHSCT for multiple sclerosis is available in some private clinics in the UK and on the NHS, albeit in a very small number of centres with limited eligibility. The treatment is aggressive, still largely experimental worldwide, and carries an estimated mortality rate of one in 330.
Why though, is stem cell treatment being offered in this way for multiple sclerosis (MS) in the absence of similar approaches for other neurological conditions?
“In MS the condition has a clear immune basis, so it makes much more logical sense to do bone marrow transplants as a way of treating the disease,” explains Roger Barker, a clinical neuroscientist at the University of Cambridge. “In neurodegenerative disorders [such as Parkinson’s], there is no such evidence, so no logic to doing this.” And despite the reasonable promise of using stem cell transplants for multiple sclerosis, many patients have been left disappointed with the results – as the BBC’s Caroline Wyatt reported recently in her quest to treat her own MS.
 Getty Images
Getty ImagesSome patient feel they simply don’t have time to wait for the culmination of good evidence from protracted clinical trials. Take this fundraising plea from a patient with ALS, a condition in which half of patients die within three years of their first symptoms:
“I am down to 32% of breathing, can't talk and loosing (sic) control of my hands and legs. I have where a breathing mask for 12-14 hours a day... PLEASE HELP!”
Doesn’t the patient who is “down to 32% of breathing” have a right to try anything that might save them, crowdfunding to do so, even if that treatment is administered an unregulated clinic? Barker is concerned that it’s this vulnerability that is being exploited, citing the potential risks, including tumour formation.
But he also believes that legitimate stem cell research will suffer. “If it goes wrong, the regulators may ban such therapies for times to come based on the belief that these clinics offer essentially the same therapies as centres which have slowly worked towards clinical trials through proper rational approaches,” says Barker.
Although regulators must play a role in tandem with cross-border partnerships, there is a growing consensus that crowdfunding platforms should take responsibility, too. Campaigns for treatments that are unsafe or lacking evidence continue to raise millions of dollars.
Protecting patients
It’s true that these platforms can empower patients to explore options, maintain hope, and cover insurance gaps, while enabling families and friends to extend their support. But shouldn’t they also ban bad actors and halt the spread of misinformation (campaigns are shared hundreds of thousands of times across social media)?
Not necessarily, suggested a GoFundMe statement to Gizmodo earlier this year: “While we hope to be a helpful resource for personal fundraising, we believe it is not our place to tell them what decision to make.” After a call for crowdfunding sites to rigorously vet cancer appeals to protect patients from unproven or dangerous treatments (such as “ozone therapy” and vitamin infusions), GoFundMe has banned users from seeking donations for treatment at certain clinics month and now report they are actively evaluating fears around certain stem cell campaigns.
“With these new concerns being raised surrounding certain stem cell clinics, we are taking a thoughtful approach to addressing stem cell campaigns while continuing to provide a safe and secure place for people to fundraise for their needs and causes. We are reaching out to experts and medical regulatory authorities in the space to understand the latest regulatory developments and how these developments affect our customers”, they said in a statement.
When presented with similar concerns, JustGiving previously stated: “We don’t believe we have the expertise to make a judgment on this.” In an email to the BBC, they asserted that they ensure that all the crowdfunding pages obey the legal requirements and assert that “the safety and wellbeing of people using our platform, whether they’re raising funds or donating to a cause, is always our priority”.
Tree of Hope, a UK crowdfunding organisation and children’s charity, claim a different approach. Their medical committee takes advice on campaigns from the UK Stem Cell Foundation. “Families turn to Tree of Hope when all other options have been exhausted,” says Lee Vallins, deputy chief executive and head of family support at the charity. “We work with some amazing, though often desperate parents and ensure we work through options with them, at their pace.” But although they have supported a number of families to crowdfund for stem cell transplants, there are safeguards in place.
“We readily spend time with parents calling us seeking advice on this type of therapy and we quite often do refuse an application if parents are unwilling to consider recognised clinical trials or alternative options to the treatment,” says Vallins. “Whilst not one of the larger crowdfunding organisations, we certainly strive to be one of the most ethical through our checks and measures throughout the process.”
Hunting for hope
Jay Shetty eventually received a two-hour infusion of stem cells through a cannula in his arm at Duke University. What were Shilpa’s expectations? “I knew it wasn’t a cure, I knew he wasn’t going to come out of it walking and running. But I thought at least Jay would be able to sit up in six months’ time, to be honest. Unfortunately, that hasn’t happened,” she says. “We haven’t seen any dramatic changes but he is not as spastic, he is more aware, for us a family we think it’s quite big. It’s a sort of foundation for all the physiotherapy.”
But was the stem cell therapy responsible for this improvement? Perhaps Jay would have acquired more skills as he grew up anyway? “It’s difficult to pinpoint because we have been doing therapy for a long time,” says Shilpa.
To date, stem cell studies on cerebral palsy at Duke University Medical Centre led by Joanne Kurtzberg, haven’t quite lived up to expectations although work is ongoing. In 2017, 63 children with cerebral palsy were randomised to treatment (a single infusion of cord blood) or placebo. Disappointingly, the researchers found no change in the trial’s primary endpoint: motor function one year after baseline infusion. They did report better outcomes at higher doses (highlighted in some media coverage) but Paul Knoefler at the UC Davis School of Medicine isn’t persuaded. “Based on the small study size, a high-degree of variability within samples in the same groups, changes in the placebo group from what was expected, and the modest nature of the possible differences with the higher dose relative to placebo, I’m not convinced the reported effect was meaningful,” he says. He also tells me that along with a study from the Duke group on autism, these results “don’t suggest a strong positive effect of umbilical cord cells for paediatric neurological conditions”.
Cells4Life, the cord blood stem cell bank that supported Jay’s fundraising, still state on their website that “the trials at Duke have shown cord blood can reverse the symptoms of cerebral palsy”. (Cells4Life state their mission is to “store every baby’s cord blood”. Their pricing varies between £1,495 ($1,816) and £2,090 ($2,538) with an additional annual storage fee.)
The Shettys remain undeterred. “If we found a match and if Duke open a similar trial I am more than happy to pay for it,” says Shilpa. “If we have money, we will just keep doing it again and again to be honest. In Jay’s case there are a lot of blank spaces in his brain and he needs new cells.”
Meanwhile, she and other parents will continue to scour the internet late at night, searching for anything might help their children, hunting for hope, calling out for a cure. As long as they do so, stem cell clinics will promise to answer their call.
--
Jules Montague is a writer and neurologist in London. Her first book, Lost and Found, explores what remains of the person when the pieces of their mind go missing - from dementia and brain injury to sleep disorders and multiple personality disorder. Her second book, The Diagnosis Cure, will be published next year and explores how medical diagnosis is deeply tainted by the forces of commerce, imperialism, and sexual discrimination.
If you liked this story, sign up for the weekly bbc.com features newsletter, called “The Essential List”. A handpicked selection of stories from BBC Future, Culture, Capital, and Travel, delivered to your inbox every Friday.
