Cancer: The mysterious miracle cases inspiring doctors

A few patients have made rare and unexpected recoveries leaving doctors scratching their heads, says David Robson. Can these cases provide vital clues for tackling cancer?
It was a case that baffled everyone involved. The 74-year-old woman had initially been troubled by a rash that wouldn’t go away. By the time she arrived at the hospital, her lower right leg was covered in waxy lumps, eruptions of angry red and livid purple. Tests confirmed the worst suspicions: it was carcinoma, a form of skin cancer.
The future looked bleak. Given the spread of the tumours, radiotherapy would not have been effective; nor could the doctors dig the tumours from the skin. Amputation was perhaps the best option, says Alan Irvine, the patient’s doctor at St James’ Hospital, Dublin – but at her age, she was unlikely to adapt well to a prosthetic limb. After a long and frank discussion, they decided to wait as they weighed up the options. “We had a lot of agonising for what to do,” says Irvine.
Then the “miracle” started. Despite receiving no treatment at all, the tumours were shrinking and shrivelling before their eyes. “We watched for a period of a few months and the tumours just disappeared,” says Irvine. After 20 weeks, the patient was cancer-free. “There had been no doubt about her diagnosis,” he says. “But now there was nothing in the biopsies, or the scans.”
Somehow, she had healed herself of arguably our most feared disease. “Everyone was thrilled, and a bit puzzled,” Irvine says, with some understatement. “It shows that it is possible for the body to clear cancer – even if it is incredibly rare.”
The question is, how? Irvine’s patient believed it was the hand of God; she had kissed a religious relic just before the healing set in. But scientists are instead looking to the underlying biology of so-called “spontaneous regression” to hunt for clues that could make these rare cases of self-healing more common. “If you can train the body to do this on a broader scale, you could have something that’s very widely applicable,” says Irvine.
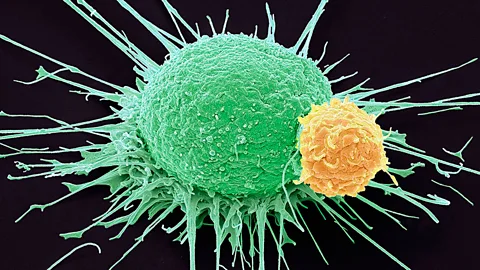
In theory, our immune system should hunt out and destroy mutated cells before they ever develop into cancer. Occasionally, however, these cells manage to sneak under the radar, reproducing until they grow into a full-blown tumour.
By the time the cancer has reached the attention of doctors, unaided recovery is highly unlikely: overall, just one in 100,000 cancer patients are thought to shed the disease without treatment.
Disappearing act
Within those scant reports, though, there are some truly incredible stories. A hospital in the UK, for instance, recently reported the case of a woman who had experienced long-lasting fertility problems. She then discovered that she had a tumour between her rectum and her uterus, but before doctors could operate, she finally conceived. All went well and a healthy baby was delivered – only for the doctors to find that the cancer had mysteriously vanished during the pregnancy. Nine years later, she shows no sign of relapse.

Similarly spectacular recoveries have now been recorded in many different kinds of cancer, including extremely aggressive forms like acute myeloid leukaemia, which involves the abnormal growth of white blood cells. “If you leave the patient untreated, they usually die within weeks, if not days,” says Armin Rashidi at Washington University in St Louis. Yet he has found 46 cases in which acute myeloid leukaemia regressed of its own accord, although only eight avoided a relapse in the long term. “If you find a random oncologist and ask if this can this happen, 99% would say no – it makes no sense,” says Rashidi, who worked with colleague Stephen Fisher on the paper.
Agonising wait
In contrast, dramatic recoveries from a childhood cancer called neuroblastoma are surprisingly frequent – offering some of the best clues about what might trigger spontaneous remission. This cancer arises from tumours in the nervous system and hormonal glands. If it then spreads, or metastasises, it can lead to nodules on the skin and growths in the liver, with swelling in the abdomen that makes it difficult for the infant to breathe.

Neuroblastoma is very distressing, yet it can sometimes disappear as quickly as it came, even without medical intervention. In fact, for infants less than one year old, regression is so common that doctors tend to avoid starting chemotherapy immediately, in the hope that the tumour will shrink by itself. “I can remember three cases with rather impressive skin metastases and an enlarged liver, but we literally just observed them – and they did well,” says Garrett Brodeur at the Children’s Hospital of Philadelphia.
The decision to sit and observe can be difficult, though: although the chance to avoid harrowing treatment comes as a relief to some parents, others find inaction and helplessness difficult to stomach. The agony of that period is one of the reasons that Brodeur wants to understand the mechanisms behind the cancer’s vanishing act. “We want to develop very specific agents that might initiate regression – so we don’t need to wait for nature to run its course or for ‘god’ to decide,” he says.
Vital clues
So far, Brodeur has some strong leads. For instance, unlike other nerve cells, the cells in neuroblastoma tumours seem to have developed the ability to survive without “nerve growth factor” (NGF) – allowing them to flourish in the wrong parts of the body where NGF is absent. Spontaneous remission may be triggered by a natural change in the neuroblastoma tumour cells, perhaps involving the cell receptors that NGF binds to. Whatever the change is, it might mean that the cells can no longer survive without the essential nutrient.

If so, a drug that targets those receptors could kick-start recovery in other patients. Brodeur says that two drug companies already have some candidates, and he hopes trials will begin soon. “It would selectively kill tumour cells that are sensitive to this pathway, so it could spare patients from chemotherapy, radiotherapy or surgery,” he says. “It wouldn’t make them sick or their hair fall out, or cause their blood cell count to fall.”
Friendly fire
Unfortunately, unexpected recoveries from other kinds of cancer have been less well studied, perhaps because of their rarity. But there are some clues, and they could come from the pioneering work of a little-known American doctor more than 100 years ago.
It was the late 19th Century, and William Bradley Coley was struggling to save a patient with a large tumour in his neck. Five operations had failed to eradicate the cancer. Then the patient caught a nasty skin infection with a scorching fever. By the time he’d recovered, the tumour was gone. Testing the principle on a small number of other patients, Coley found that deliberately infecting them with bacteria, or treating them with toxins harvested from microbes, destroyed otherwise inoperable tumours.
Unfortunately, unexpected recoveries from other kinds of cancer have been less well studied, perhaps because of their rarity. But there are some clues, and they could come from the pioneering work of a little-known American doctor more than 100 years ago.
It was the late 19th Century, and William Bradley Coley was struggling to save a patient with a large tumour in his neck. Five operations had failed to eradicate the cancer. Then the patient caught a nasty skin infection with a scorching fever. By the time he’d recovered, the tumour was gone. Testing the principle on a small number of other patients, Coley found that deliberately infecting them with bacteria, or treating them with toxins harvested from microbes, destroyed otherwise inoperable tumours.

Could infection be the key to stimulating spontaneous remission more generally? Analyses of the recent evidence certainly make a compelling case for exploring the idea. Rashidi and Fisher’s study found that 90% of the patients recovering from leukaemia had suffered another illness such as pneumonia shortly before the cancer disappeared. Other papers have noted tumours vanishing after diphtheria, gonorrhoea, hepatitis, influenza, malaria, measles, smallpox and syphilis. What doesn’t kill you really can make you stronger in these strange circumstances.
It’s not the microbes, per se, that bring about the healing; rather, the infection is thought to trigger an immune response that is inhospitable to the tumour. The heat of the fever, for instance, may itself render the tumour cells more vulnerable, and trigger cell suicide. Or perhaps it’s significant that when we are fighting bacteria or viruses, our blood is awash with inflammatory molecules that are a call to arms for the body’s macrophages, turning these immune cells into warriors that kill and engulf microbes – and potentially the cancer too. “I think the infection changes the innate immune cells from helping the tumours to killing them,” says Henrik Schmidt at Aarhus University Hospital in Denmark. That, in turn, may also stimulate other parts of the immune system – such as our dendritic cells and T-cells – to learn to recognise the tumorous cells, so that they can attack the cancer again should it return.

Schmidt thinks that understanding the process of spontaneous remission is vital, since it could help refine the emerging class of “immunotherapies” that hijack our natural defences to combat cancer. In one treatment, for instance, doctors inject some cancer patients with inflammatory “cytokines” in order to kick the immune system into action. The side effects – such as high fever and flu-like symptoms – are typically treated with drugs like paracetamol, to improve the patient’s comfort.
But given that the fever itself may trigger remission, Schmidt suspected that the paracetamol might sap the treatment’s potency. Sure enough, he has found that more than twice as many patients – 25% versus 10% – survive past the two-year follow-up, if they were instead left to weather the fever.
There could be many other simple but powerful steps to improve cancer treatment inspired by these insights. One man experienced spontaneous remission after a tetanus and diphtheria vaccination, for instance – perhaps because vaccines also act as a call to arms for the immune system. Along these lines, Rashidi points out that a receiving standard vaccine booster – such as the BCG jab against tuberculosis – seems to reduce the chance of melanoma relapse after chemotherapy.
Catching a cure
Others are considering a far more radical line of attack. For instance, one approach aims to deliberately infect cancer patients with a tropical disease.

The technique, developed by American start-up PrimeVax, involves a two-pronged approach. It would begin by taking a sample of the tumour, and collecting dendritic cells from the patient’s blood. These cells help coordinate the immune system’s response to a threat, and by exposing them to the tumour in the lab, it is possible to programme them to recognise the cancerous cells. Meanwhile, the patient is given a dose of dengue fever, a disease normally carried by mosquitoes, before they are injected with the newly trained dendritic cells.
Under the supervision of doctors in a hospital, the patient would begin to develop a 40.5C fever, combined with the widespread release of inflammatory molecules – putting the rest of the immune system on red alert. Where the tumour was once able to lurk under the radar, it should now become a prime target for an intense attack from the immune cells, led by the programmed dendritic cells. “Dengue fever crashes and regroups the immune system, so that it is reset to kill tumour cells,” says Bruce Lyday at PrimeVax.
Infecting vulnerable patients with a tropical illness may sound foolhardy, but dengue fever is less likely to kill the average adult than the common cold – making it the safest choice of infection. Importantly, once the fever has subsided, the programmed immune cells will remain on the lookout for the tumour, should it reappear. “Cancer is a moving target. Most therapies attack from just one side – but we’re trying to put it in a lose-lose situation, now and in the future,” says Lyday.
No one could fault the ambition behind this kind of therapy. “Our mission is to replicate spontaneous remission in as standardised way as possible,” says Lyday’s colleague Tony Chen. Even so, they are keen to emphasise that their idea is still at a very early stage of development – and they cannot know how it will play out until they begin a clinical trial. The first tests, they hope, will begin with advanced melanoma patients, perhaps by the end of the year.
Clearly, caution is necessary. As Irvine points out: “Spontaneous remission is a little clue in a big complicated jigsaw.” But if – and that is a massive if – they succeed, the implications would be staggering. A rapid, relatively painless recovery from cancer is now considered a miracle. The dream is that it might just become the norm.
